By Katherine Ladny Mitchell
In 1928, Professor Alexander Fleming was sorting through bacterial cultures when he noticed some mold in a petri dish. Upon closer observation, he saw no bacteria had grown around the mold. Had the mold produced something to destroy the bacteria? This question was the germ from which he developed penicillin – the famous antibiotic we know for curing diseases like pneumonia and blood poisoning.
Today, more than 100 antibiotics exist to fight infections by interfering with bacteria’s ability to replicate, construct proteins, or create cell walls. In the past century, they have saved millions of lives. And yet, these medications have their limitations. Ever wondered what they can and can’t do? We’ve got the answers here.

Most of us understand antibiotics as strong medicines used to treat infections. But what you might not know is that they can only do one thing: treat infections brought on by bacteria. You can’t just use any antibiotic for any infection – you have to match the right medication to the right bacteria. This is why doctors often use lab tests to identify bacteria before writing you a prescription.
Here are a few cases where an antibiotic might be appropriate, depending on the nature of your symptoms:
Strep Throat. If you have strep throat, which is caused by streptococcal bacteria, white spots in your throat can indicate the presence of bacteria. Your doctor will swab your throat if he or she suspects you have strep. A simple test can confirm the diagnosis and your need for an antibiotic.
Pneumonia. If you have pneumonia your doctor may test your blood and sputum (liquid coughed up from the lungs) to identify the extent and cause of the infection. If tests reveal a bacterial cause, your doctor will prescribe the appropriate antibiotic.
Ear Infection. While some ear infections are bacterial, the large majority will not require an antibiotic. If your pain grows severe and/or is accompanied by a fever, you doctor may prescribe one. However, he or she may puncture the eardrum and culture the fluid to check for bacteria first.
Persistent or Severe Sinus Infection. Most sinus infections are not caused by bacteria and therefore will not require antibiotics. However, a small percentage may become bacterial infections after 7 to 10 days. In a true bacterial sinus infection, symptoms will be severe and persistent. “You will have nasal discharge resembling puss, severe sinus pressure, upper molar pain,
and fever,” says Dr. Brian Daily, family medicine physician with Professional Park Associates.




Osteopathic Physician,
Parkridge Medical Group – Diagnostic Center
Contrary to a common misconception, antibiotics can’t treat viral sicknesses like the flu or a cold. “Viruses, as opposed to bacteria, cause the vast majority of upper respiratory infections,” says Dr. Nathan Hartgrove, an osteopathic physician with Parkridge Medical Group – Diagnostic Center. Translation? In most cases, an antibiotic will have no ability to fight your symptoms of congestion, sore throat, headache, and fatigue.
If you contract a cold or bronchitis as an adult without other health problems, your body should be able to recover on its own. Get extra rest, drink copious amounts of fluid, and treat your symptoms with over-the-counter cold and flu medications. Perhaps most importantly, give yourself permission to be sick. “We should not underestimate the potential for healing with conservative approaches,” says Hartgrove. “Our bodies are amazing creations. God has given us the ability to recover from things we encounter daily.”
During this time, you may be tempted by “magic pill” remedies and grow concerned if you aren’t better after a week or two. Be patient – it’s normal for healing to take time. “It’s hard for our American culture to accept that people may need a significant amount of time off,” says Dr. Daily. “We don’t let ourselves or others be sick, or give our bodies time to recover. Addressing this culture of shame is one of the first steps we can take to make progress.”
Finally, if you happen to catch the latest bug, be wary of asking your doctor for an antibiotic. Beyond not being able to help you, taking an antibiotic when you don’t need it may even hurt you. Read on to learn more.


Most antibiotics work in one of two ways. They either 1) kill the bacteria causing the infection, or 2) stop it from multiplying and give your immune system a chance to kill it on its own. In either case, they get the job done by attacking the invader bacteria making you sick. Like an army, they go into your body, find the bad guys, and either bring them down or contain them.
But what if you release antibiotics into your body and they have no “bad guys” to chase? Faced with no enemy, these medications may attack your body’s healthy bacteria instead. “When you take antibiotics inappropriately, you expose the normal flora of your body – the healthy bacteria that help you digest food and perform other vital functions – to something which threatens to eradicate them,” says Dr. Hartgrove.
Another, and even more dangerous thing that can happen, is that you may develop antibiotic resistance. Antibiotic resistance is when the bacteria in your body are no longer sensitive to an antibiotic. Here’s how it works: when you take antibiotics inappropriately, bacteria that already exists in your body can mutate to protect itself from the drug. “Bacteria are very smart,” says Dr. Daily. “They have an extraordinary ability to adapt quickly to survive.”
Any bacteria that survives the antibiotic can multiply and pass on antibiotic-resistant properties to other bacteria. Eventually, it makes the medication useless when you need it. Your doctor may then have to prescribe several alternatives before finding an effective one. Sometimes, people even run out of options.
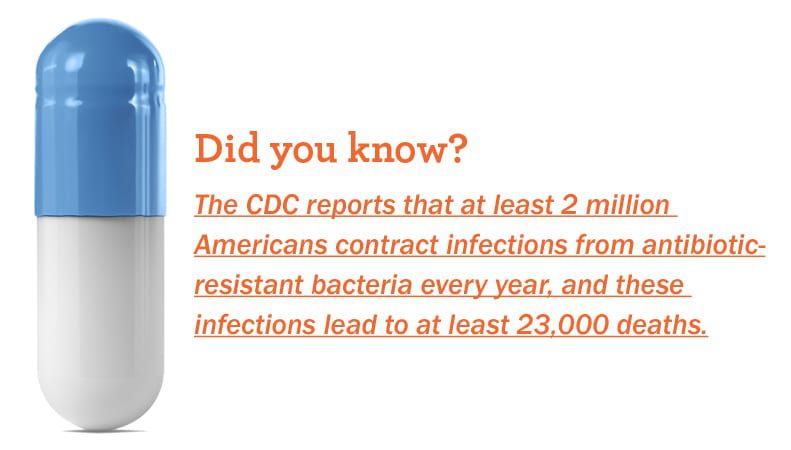
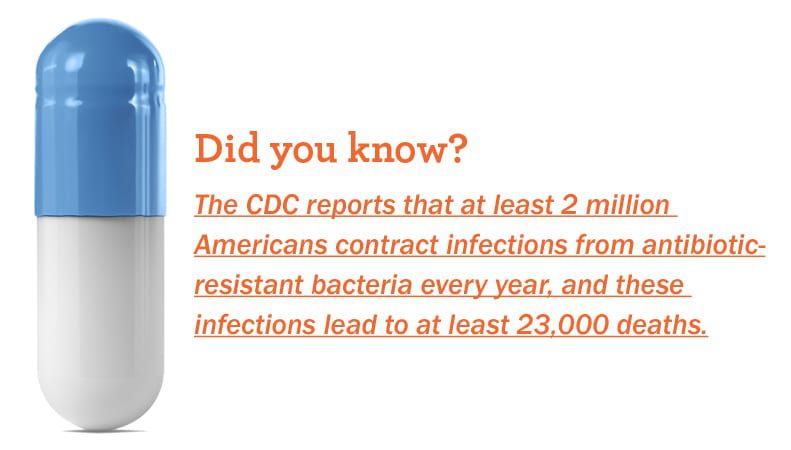


Antibiotic-resistant bacteria can lead to more severe sicknesses, longer recuperation times, more trips to the doctor or time at the hospital, and costly additional treatments. According to Choosing Wisely, an initiative of the American Board of Internal Medicine (ABIM) Foundation, treating an antibiotic-resistant blood infection incurs around $40,000 in extra medical expenses per patient. This translates to about $20 billion in annual treatment costs.
Worldwide, antibiotic resistance has become a public health crisis, according to Dr. Daily. “As of recent history, we now have resistance to every type of antibiotic that exists today,” he says. “The CDC says it’s like living in the ‘40s, because even though we have antibiotics, we can’t guarantee they will work. If you get sick with a bacterial infection, it’s possible you may just have to weather it out like people used to.”




Family Medicine Physician
Professional Park Associates
To protect yourself from the consequences of antibiotic resistance, begin by educating yourself about when antibiotics are and aren’t appropriate. Showing up at the doctor to demand antibiotics when you have a virus is a lose-lose situation. If your doctor gives you one, it won’t help you get better and you may develop antibiotic resistance. If you aren’t given one, the situation will simply add to your frustration.
“Education is the most important first step,” says Dr. Daily. “The CDC has a major campaign going to lessen the use of antibiotics. Often, I offer their pamphlets and materials to my patients. I also have a poster on the back of my door – anything to help people understand the danger of antibiotic resistance.”
Second, if your doctor does prescribe you an antibiotic, follow all medication instructions to the letter. Take the full number of doses – if you stop taking an antibiotic before you’ve finished an entire course, some of the “bad” bacteria may survive and become resistant.
Finally, do not share your antibiotics with anybody else or use another person’s medication. Following these tips will help protect our medications’ effectiveness and best serve you – and everyone else – for years to come.