By Alice Gilmore
You’ve heard of statins. Around since 1987, these lipid-lowering medications have continued to rise in popularity as they’ve been proven to lower cardiovascular disease in high-risk individuals. And just under four years ago, the guidelines for prescribing them broadened even more. Now, individuals who have either suffered from a heart-related event in the past or are at risk for one in the next 10 years are encouraged to consider taking a statin. With one in four U.S. adults receiving a prescription, statins are the most common treatment given out by doctors today. Read on to learn six facts you might not know about these life-changing drugs.


BACKGROUND: In order to understand statins, it’s important to first understand cardiovascular disease. The term cardiovascular disease refers to conditions in which narrowed or blocked blood vessels or arteries lead to heart attack, chest pain, or stroke. Narrowed vessels and arteries are a result of plaque buildup. Plaque forms when cholesterol, combines with triglyceride (fat), calcium, and other substances in the blood.
Cholesterol is produced in the liver and is essential to the body, as it helps absorb fats and fat-soluble vitamins. It also aids in the creation of vitamin D, estrogen, testosterone, and cortisol. Triglycerides can be broken down to create energy for the body. According to Dr. Gary Olson, a cardiologist with Hamilton Cardiology Associates, “Both cholesterol and triglycerides are considered fats, and therefore cannot circulate freely in the blood unless paired with proteins to form lipoproteins. These carrier proteins give the fats their good or bad characteristics.” Cholesterol travels through the body as one of the following: high-density lipoprotein (HDL), low-density lipoprotein (LDL), and very-low-density lipoprotein (VLDL). HDL is considered good cholesterol, and high numbers are good for heart health. LDL and VLDL are considered bad cholesterol, meaning high numbers can lead to heart events. Ultimately, abnormal lipoprotein levels can lead to atherosclerosis, or the hardening or narrowing of the arteries that leads to heart disease.
1. Statins are used to lower your cholesterol.
Statins are a class of medications that block the liver’s production of bad cholesterol and triglycerides (fat), while improving production of good cholesterol.
Dr. Richard Pigg, a primary care physician with CHI Memorial notes, “Low-density lipoprotein (LDL) is considered bad cholesterol, while high-density lipoprotein (HDL) is considered good. LDL cholesterol contributes to fatty buildup and plaque in the arteries, which can lead to heart attack or stroke.”
Statins work by inhibiting the enzyme, called HMG-CoA reductase, that controls the production of cholesterol. Cholesterol levels are directly correlated with a person’s risk of experiencing a heart event. When cholesterol levels are lowered, so too is an individual’s risk for heart attack or stroke.
2. Statins have other benefits, too.
Statins are considered the primary treatment to lower an individual’s risk for heart attack or stroke. Not only do they lower cholesterol, they also have numerous other health benefits, as well. One benefit is their ability to reduce inflammation in the artery walls caused by oxidation. When oxygen is metabolized, it produces “free radicals” that cause damage to cell membranes and other structures. Statins can also reduce the risk of narrowed arteries by keeping the muscle lining of the arteries smooth and reducing fibrin (protein involved in blood clot formation) deposits.
3. Statins are not free of side-effects.
Of course, with any pharmaceutical, negative side effects are possible, and statins are no exception. Although some patients report digestive problems and a degree of mental fuzziness, muscle pain is the most common complaint. In fact, nearly 30% of statin users notice muscle soreness, tiredness, or even weakness. While most describe the muscle fatigue as an inconvenience, some report that the effect is so extreme that completing simple, everyday activities becomes difficult. Patients who experience this type of discomfort often find relief by switching to another type of statin. And according to Dr. Olson, “Patients who seem to have trouble tolerating statins due to muscle aches may benefit from taking one of the longer acting statins every other day or three days a week.”
Less likely, but still a risk that your healthcare provider will keep an eye on, is rising blood sugar levels. If you are susceptible to this side effect, prolonged statin use could contribute to liver damage and even the development of type 2 diabetes. The risk of this is small, but still significant enough that the Food and Drug Administration (FDA) feels it must make note of it on the prescription label.
Although not everyone who takes a daily statin will experience negative side effects, some are more prone to experience them than others. Gender, age, existing liver or kidney disease, small body frame, excessive alcohol consumption, and the use of other prescribed medications may all contribute. For example, women in general and anyone over the age of 65, may be more susceptible to negative side effects. “Your clinician will always weigh the risks and benefits associated with placing you on a statin,” says Dr. Pigg. “If your doctor determines a statin is right for you, he or she will monitor your progress and make adjustments as needed.”


4. Statins are widely used.
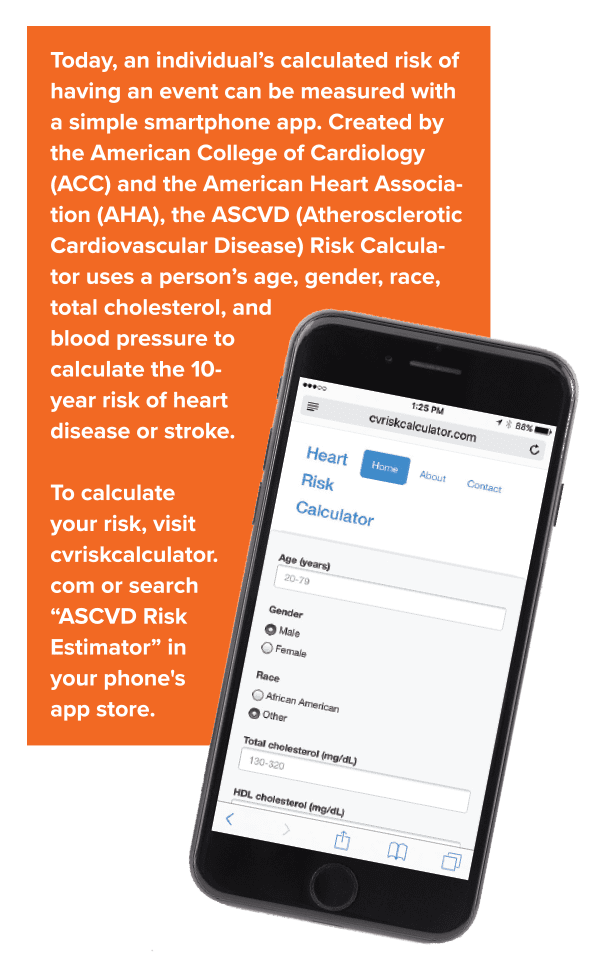
Statins are prescribed to one in four Americans over age 45, often in people who appear healthy. What’s the reasoning behind this? A person’s risk of having a heart-related event, like a stroke or heart attack, plays a major role. According to Dr. Olson, “The current guidelines recommend we assess people’s risk of having a heart-related event in the next 10 years. If the risk calculates to 7.5% or higher, statins are recommended.”
Those who have experienced an event in the past will always remain at risk for another. Therefore, in addition to lifestyle changes, they will be placed on statins as a secondary prevention. “Statins are indicated as primary prevention for individuals with more than three risk factors, who are considered at high risk for developing cardiovascular disease. These factors include being male, obese, having high cholesterol or diabetes, using tobacco, or having a male relative younger than 55 or female relative younger than 65 who has experienced a heart attack. Anyone who has already had a heart attack should be on a statin as secondary prevention,” says Dr. Eugene Ryan, an internist with Parkridge Medical Group.


5. Guidelines for prescribingstatins have changed.
In 2013, the American Heart Association (AHA) and the American College of Cardiology (ACC) updated their cholesterol treatment guidelines with the intention of preventing more heart attacks and strokes. The previous guidelines focused only on specific target levels of LDL, and statins were recommended for anyone above the target.
The new guidelines eliminated the LDL targets, and instead identified four major patient groups that would benefit from statins. Those groups include patients with cardiovascular disease, patients with an LDL level of 190 mg/dL or higher, patients age 40-75 who have type 2 diabetes, and patients with a 7.5% or higher risk of developing cardiovascular disease in the next 10 years. Now factors like weight, blood pressure, lifestyle, and family history play a larger role. “The original guidelines focused too much on specific target numbers. Now patient care can be more individualized,” says Dr. Ryan.
You and your doctor may decide that statins are a needed part of your overall cardiac health, but small lifestyle changes can be helpful, too. “Before considering the use of statins to lower cholesterol, patients should first modify their diet and exercise routines,” says Dr. Ryan. Consider starting the day with a bowl of oatmeal or another whole grain like barley or farro. Just two servings of oats a day can lower bad cholesterol by more than 5% in six weeks. And if you enjoy a glass of wine with your dinner, forgo the Pinot Grigio or Chardonnay and choose a red instead, perhaps one made of high-fiber Tempranillo grapes. Exercise daily and avoid refined sugars. Spinach, strawberries, sweet potatoes, okra, and eggplant are some smart food choices your heart will appreciate.
The best way to determine if statins might be right for you is to visit your doctor and get your cholesterol tested. These little pills can make a big difference when it comes to your heart health.

