Disorders and Diseases Affecting the Peripheral Blood Vessels
Congestion, roadblocks, narrow lanes: From slowdowns to standstills, these are the makings of a traveler’s nightmare. But what happens when the same conditions occur within the human body?
What Is Vascular Disease?
Vascular disease is a form of cardiovascular disease primarily affecting the blood vessels, so to fully understand it, it’s helpful to know a little about how blood flows through the body, which has two main parts. Part one is pulmonary circulation, a loop of blood vessels that carries blood from the heart to the lungs, where it picks up oxygen and promptly circles back to the heart. The heart then pumps the oxygenated blood through the systemic circulation – part two of the circulatory system – which supplies blood to every part of the body, except for the lungs.
Blood vessels are one-way streets: arteries carry oxygen-rich blood away from the heart; once the tissues and organs have used the oxygen, veins carry oxygen-depleted blood back to the heart. The blood is then sent to the lungs to refuel with oxygen, and the process repeats.
Peripheral Vascular Disease, or PVD, refers to diseases in any of the blood vessels outside of the heart arteries and veins. The legs and feet are most commonly affected, thus the name peripheral vascular disease.
Vascular disease can be either functional or occlusive. A disease that is “functional” involves temporary spasms of the blood vessels; it doesn’t involve problems with the blood vessels themselves.
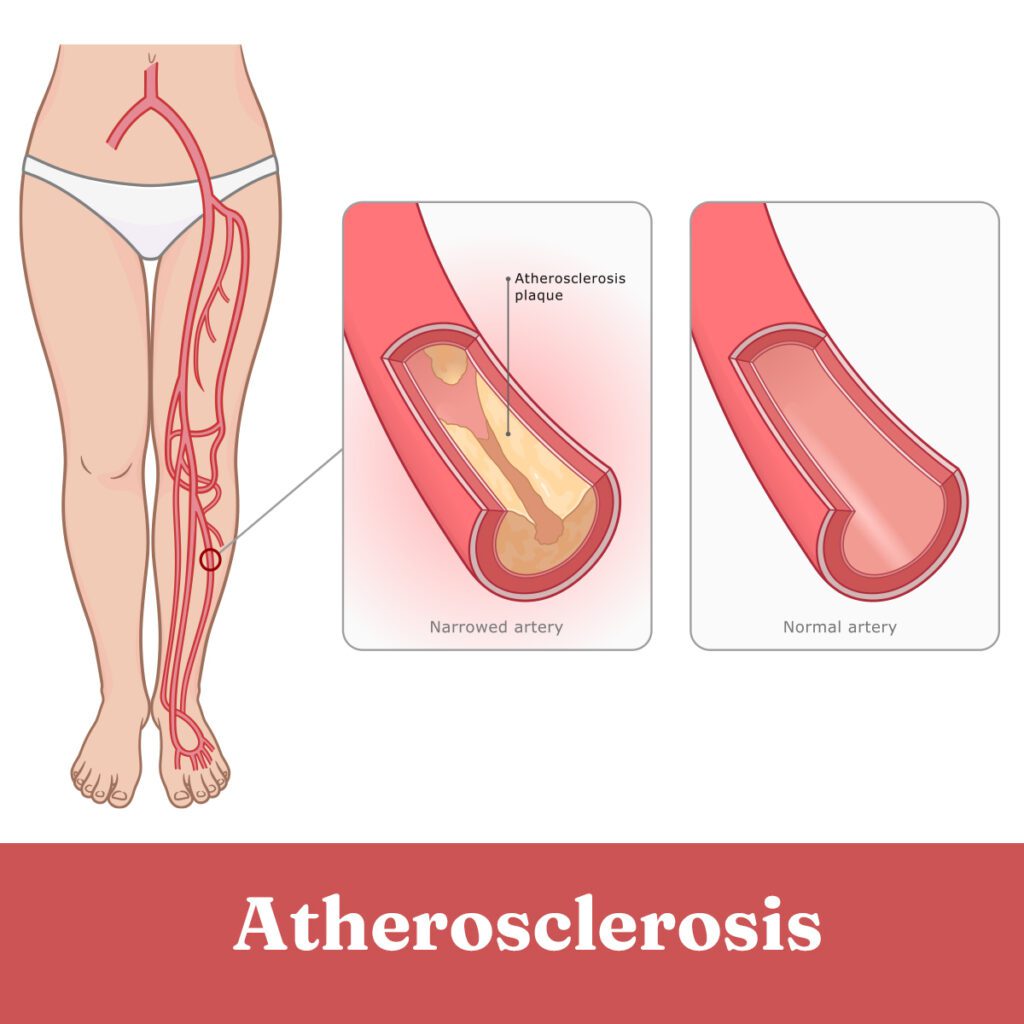
When people talk about PVD, they are generally referring to peripheral arterial disease (PAD), a condition when atherosclerosis affects the peripheral arteries. More often than not, PAD is found in the legs, but the arteries in the arms can also be at risk.
Atherosclerosis is the process in which plaque builds up inside the arteries. A sticky substance, plaque consists largely of fat, cholesterol and calcium. It has a bad reputation, and rightly so. When plaque collects in the arteries, it hardens, narrowing or blocking the vessels. In its most severe form – and if left untreated – PAD can result in tissue death and require amputation. Usually, that can be avoided by managing risk factors and seeking treatment at the first sign of a problem.
PAD Symptoms and Risks
Heart disease tends to take center stage when it comes to blood vessel troubles. But PAD certainly holds its own: in the U.S., between 8 to 10 million people have the disease. Risk of PAD increases with age, diabetes, smoking, being overweight or obese, high blood pressure, high cholesterol, lack of exercise, genetics and race (some vascular diseases are more prominent in African Americans). “The two major risk factors are diabetes and smoking,” says Dr. Brian H. Negus, a cardiologist with The Chattanooga Heart Institute at Memorial. “People could cut rates of PAD 25 percent by quitting smoking alone.”
About half of people diagnosed with PAD are symptom-free. Those who are symptomatic typically complain of a dull, cramping pain, or a heaviness, tightness or tiredness in the leg muscles. Frequently, pain occurs with movement or exercise – times when the body demands additional oxygen and nutrients. If the vessels are narrowed or blocked, they have difficulty supplying the necessary blood. That results in “intermittent claudication” – pain that comes with movement and disappears upon resting. Complete blockage of the vessels also can cause pain at night.
“People may be asymptomatic for years,” says Dr. Negus. “Some will get intermittent claudication in the legs when they walk that is relieved with rest, so they’ll limit their activity, thinking ‘I’m getting old.’ It’s a good idea to find out if it’s an arteriosclerosis problem, because the same things that cause coronary artery disease cause [PAD] in the legs.”
“Most people with peripheral artery disease will actually die of the coronary artery disease. They gradually decrease their activity, and they don’t put enough stress on their heart and may not notice symptoms.”
According to the Mayo Clinic, other PAD symptoms that occur in the legs include:
- Muscle pain and cramping, usually in the calf
- Coldness in the leg or foot
- Weakness or numbness
- Sores that won’t heal
- Hair loss or slow hair growth
If you experience any of these PAD symptoms, consult your primary care doctor to discuss if you may have PAD.
PAD Treatment Options
While there is currently no cure for PAD, the symptoms can be managed and treated. Oftentimes, the goal of treatment is to reduce leg pain to make exercise more comfortable and to improve artery health to decrease the chance of a heart attack, stroke, and other heart-related issues.
According to the Cleveland Clinic, treatment options usually include lifestyle changes, surgeries, and different kinds of medication.
- Lifestyle Changes: To manage symptoms of PAD, most doctors recommend increasing regular exercise, eating a healthy and nourishing diet, and quitting unhealthy activities, like smoking or using tobacco.
- Surgery: There are a few different procedures that can help mitigate symptoms from PAD. In thrombolytic therapy, medicine is injected directly into the artery to dissolve a clot. With an angioplasty and stent placement, a tiny balloon on a tube, called a catheter, is inflated inside the artery to enlarge the pathway. A stent is then placed in the artery to keep it open. Lastly, patients can undergo bypass surgery. In this procedure, the doctor will take a healthy blood vessel from elsewhere in the body and create a new path for the blood to flow around the clog.
PAD Medication
For some individuals, medication may be the best method to treat PAD. There are many different medications that can be taken:
- Statins: Statins are used to lower the LDL (or “bad”) cholesterol in the body, which can reduce the risk of a heart attack or stroke. Statins also help clear plaque from the body’s arteries.
- Blood pressure medication: High blood pressure can make the body’s arteries stiff and hard, which can make it difficult for blood to flow through the arteries. A doctor may prescribe blood pressure medication to keep your blood pressure under control.
- Diabetes medication: Those with diabetes are more likely to develop PAD. Diabetes medication can help regulate an individual’s blood sugar.
- Clot prevention medication: A reduction in blood flow can contribute to clots in the body. Aspirin and other blood thinners can help prevent blood clotting.
Because each individual is different, consult your primary care provider before taking any medications to treat PAD symptoms.
Other Types of Peripheral Vascular Disease
Raynaud's (Primary and Secondary) and Buerger's
Other vascular diseases involving the peripheral arteries and veins include Raynaud’s—referred to as a phenomenon, disease, or syndrome. A functional type of vascular disease, Reynaud’s is marked by a brief episode of vasospasm, a narrowing of the arteries that reduces blood flow to the fingers and toes. The skin will sometimes turn white and then blue. When blood flow returns, the skin becomes reddened and throbs, tingles, or feels numb.
If the cause of Raynaud’s is unknown, it’s called primary Raynaud’s. If a disease or other factor is to blame, it’s called secondary Raynaud’s – a rarer and more severe condition that can entail skin sores or gangrene.
Secondary Raynaud’s is caused by conditions that directly damage arteries (think: PAD), as well as damage to nerves that control arteries. It can also be caused by rheumatoid arthritis, atherosclerosis, blood disorders, thyroid problems, and pulmonary hypertension, among others.
Secondary Raynaud’s can sometimes be linked to a history of Buerger’s disease, a type of occlusive vascular disease strongly associated with use of tobacco products. With Buerger’s, tiny vessels (arteries or veins) of the hands and feet tighten or become totally blocked. Cold hands and feet, discoloration, acute pain and intermittent claudication in the legs are all symptoms.
For both Buerger’s and Raynaud’s, there is no cure. However, you can manage the symptoms. Avoiding tobacco use and cold temperatures is recommended, and exercise can help by increasing circulation. In more severe cases, surgery may offer relief.
Aneurysms
Aneurysms are another type of vascular disease that can affect the peripheral arteries. An aneurysm is an abnormal widening or ballooning of an artery due to weakening of the vessel wall. While they often occur in the heart’s major artery – the aorta – and the brain, aneurysms are not rare in the peripheral arteries. It’s not clear exactly what causes them; some are considered congenital. High blood pressure, high cholesterol and smoking may be culprits, too. Symptoms are somewhat rare unless they rupture, an event that can be painful or fatal. CT scans and ultrasounds are used to detect aneurysms, and endovascular or open surgery generally is recommended.
Peripheral Venous Diseases
Arteries may have their fair share of potential problems, but peripheral vascular disease doesn’t discriminate. Peripheral vascular diseases that affect only the peripheral veins are called peripheral venous diseases.
Veins contain flaps, called valves, which open when your muscles contract, and close when your muscles relax. This keeps blood flowing in the right direction. Damage may prevent the valves from closing completely, so blood flows in both directions. Ultimately, this can cause pooling of blood or swelling in the veins, setting the stage for a host of potential health conditions.
Deep Vein Thrombosis
Deep vein thrombosis, or DVT, is a blood clot that forms in a vein deep within the body. DVT can be dangerous: it’s possible for the clot to break off from the location where it formed – typically in the lower leg or thigh – and travel through the bloodstream, forming a blockage in the lungs (known as pulmonary embolism). Causes of DVT include damage to the lining of a vein, slow blood flow or blood that is thicker than normal.
Swelling, pain, tenderness and discoloration at the site of the blood clot are the main symptoms of DVT, but only half of the people affected are symptomatic. Sometimes, there are no signs of the condition until the clot has traveled to the lungs.
Various tests can help diagnose DVT before it causes a serious problem. Clots can be dissolved with medications, and certain medical devices can catch clots, keeping them from making a trip to the lungs.
Chronic Venous Insufficiency
DVT can lead to other conditions, such as chronic venous insufficiency, or CVI, a relatively common form of peripheral venous disease. CVI occurs when the veins are unable to properly send blood back to the heart, resulting in the pooling of blood in the leg veins. In addition to DVT and other blood clots, CVI can be caused by vein wall weakness or an absence of vein valves since birth.
Over time, the legs may experience swelling, itching or discoloration, and skin ulcers may develop. Compression socks, movement and surgery are possible treatment options.
Varicose Veins
CVI often goes hand-in-hand with varicose veins—narled, enlarged veins that usually pop up in the legs and feet. Varicose veins are dark purple or blue, and they resemble swollen cords running through the legs. Concerns are usually more cosmetic than medical.
Of course, there are exceptions. Varicose veins may be accompanied by aching, burning, itching and in more serious cases, skin ulcers. Occasionally, they signal a higher risk of other circulatory problems. Women are more commonly affected than men, and, the condition is frequently a result of pregnancy, obesity or long periods of standing.
If you suffer from varicose veins, exercise, leg elevation and compression socks may ease pain and prevent further damage. Basic outpatient procedures can be performed to remove veins or reduce their appearance.
Prevention
Peripheral vascular disease can be complex, and it takes many forms— some more serious than others. Fortunately, medical treatment is usually available, and in many cases, it provides a complete cure.
But you can take steps to avoid peripheral vascular disease and treatment altogether. Most importantly, know what puts you at risk. If you’re prone to peripheral vascular disease—particularly peripheral artery occlusive disease—due to age or genetics, it’s all the more necessary to understand the disease and be aware of its early signs. Many risk factors can be managed, or even eliminated, through basic lifestyle changes. That includes quitting smoking, losing weight, eating well, exercising and treating high cholesterol and blood pressure.
“With PAD, walking is actually good for the legs. It’s nature’s own bypass. People can often double their walking distance just by trying,” says Dr. Negus. “It’s also important to protect your legs and feet so you don’t get wounds.”
According to Dr. Negus, a simple way to screen for PAOD is an ankle-brachial index test, which measures the blood pressure of the arm and the ankle while at rest. A normal resting ankle-brachial index is 1.0 to 1.4.
Like a traffic jam on the interstate, peripheral vascular disease can have a snowball effect—so make sure you’re in the driver’s seat. Take action by leading a healthy lifestyle and working with a trusted medical provider to prevent vascular disease, reverse damage and ultimately maintain a steady flow.
Meet the Author

Ali Lemmons, BS, Summa Cum Laude
Ali Lemmons is a graduate of the University of Tennessee at Chattanooga (UTC) where she earned a Bachelor of Science degree in Communication with a minor in computer science. While at UTC, Ali also earned the distinction of Summa Cum Laude, the Outstanding Senior Award for the communication department, and was inducted into the Kappa Tau Alpha honor society. Now, as editor/digital content specialist for CMC Media & Marketing Group, Ali leads the ideation, conceptualization, and development of numerous health, wellness, business, sports, and lifestyle articles published in print and online for HealthScope®, CityScope®, and Choose Chattanooga® magazines – premier publications serving S.E. Tennessee and North Georgia. She is also involved in content creation for Digital Smart Marketing customers and is the lead copywriter for the company’s social media sites.
