Could Your Kids be at Risk?
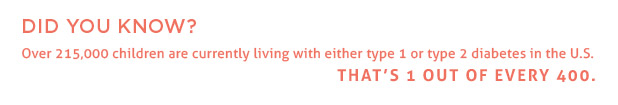
Diabetes, a chronic condition that affects how the body metabolizes sugar, is one of the most common chronic diseases found in children and young adults. In the U.S., approximately 15,600 children and adolescents are diagnosed with type 1 diabetes every year. However, the last 20 years have seen a startling rise in the number of young people diagnosed with type 2 diabetes—a form traditionally seen only in adults 40 and older. Until the 1990s, more than 95% of children who developed diabetes had type 1 diabetes. Today, depending on the population studied, anywhere between 10-50% of children diagnosed with diabetes have type 2 diabetes.
By Pamela Boaz
Why this spike in cases?
Doctors point to the obesity epidemic. Most new cases of type 2 diabetes in adolescents co-exist with being overweight or obese, and the disease is becoming increasingly prevalent in younger children with the same weight problems. In fact, the top two risk factors for the disease are: 1) obesity, and 2) a family history of type 2 diabetes. Children and adolescents who do not engage in regular physical activity, as well as those who do not eat well, have a higher risk across the board. At least 75% of children with type 2 diabetes have a parent, sister, or brother with the disease.
Is type 2 diabetes really that big of a deal?
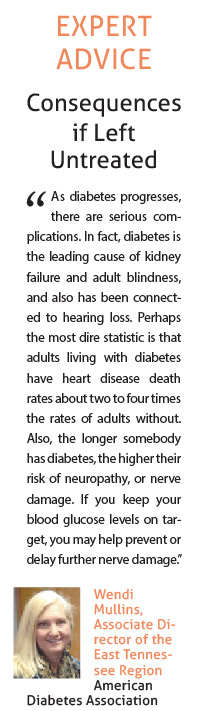
Absolutely. Here’s why: type 2 diabetes doesn’t usually exist as an isolated condition. Rather, the disease creates the potential for, and likelihood of, other serious health issues. Early diagnosis and treatment of type 2 diabetes is crucial to maintaining one’s long-term health, because if blood sugar levels remain high, they can lead to complications like:
Heart disease: High blood pressure is often an early problem resulting from diabetes. Over time, other cardiovascular issues—such as coronary artery disease and stroke—can occur as well.
Nerve damage: Another complication of diabetes is neuropathy, or nerve damage, particularly in the legs and feet. Nerve damage is the result of damage to tiny blood vessels (capillaries) that send nourishment via blood to the nerves. When the nerves lack sufficient blood, tingling, numbness, or pain can
occur.
Kidney damage: Diabetes can also injure the blood vessels that filter waste from the blood, which leads to kidney damage.
Eye damage: Blood vessels in the retina damaged by diabetes increase the risk of cataracts, glaucoma, and even blindness.
Other conditions: Diabetes can make a person more likely to have skin problems and gum disease, increase risk of Alzheimer’s disease, and even lead to hearing impairment.
So you see: bringing blood sugar levels back within a normal range may be the immediate goal of treatment, but the ultimate goal is to reduce the long-term risk of developing these serious types of complications.
How can I recognize the symptoms in my child?
While type 1 diabetes develops quickly, type 2 comes on gradually. Parents can look for four behaviors that may signal the development of type 2 diabetes in children and teens: 1) excessive urination (including sudden bed-wetting episodes), 2) increased thirst, 3) unusual fatigue, and 4) blurry vision. Parents whose child is diagnosed with diabetes often just say their child seemed “a little off,” so if you suspect something is wrong, contact your healthcare provider.
However, children and teens who are insulin resistant may not always exhibit these typical symptoms. That’s why it is perhaps more important to identify risk factors.
Because weight is among the highest risk factors for type 2 diabetes, parents who recognize that their child has an above-average body mass index (85th percentile or more) should schedule their child for testing. This is even more important if there is a family history of diabetes.
Testing usually involves a combination of blood and urine tests. An official diabetes diagnosis is made when a child’s fasting blood sugar levels reaches or exceeds 126 milligrams per deciliter.
Can type 2 diabetes be delayed?
 Often, yes—if measures like weight loss are taken seriously. Taking a proactive stance when the signs and symptoms of type 2 diabetes first appear can delay, or even prevent, the disease from developing further. Obesity, the number one risk factor for type 2 diabetes in children and young adults, can be addressed by developing healthy lifestyle habits, like:
Often, yes—if measures like weight loss are taken seriously. Taking a proactive stance when the signs and symptoms of type 2 diabetes first appear can delay, or even prevent, the disease from developing further. Obesity, the number one risk factor for type 2 diabetes in children and young adults, can be addressed by developing healthy lifestyle habits, like:
A balanced diet: An important first step is changing one’s diet. Foods high in carbohydrates, which are turned into glucose by the body, as well as foods that contain large amounts of sugar (soda, candy, pastries, etc.) should be eliminated or greatly reduced in the diet. Your doctor may also recommend a low-sodium diet to help reduce the risk of high blood pressure, a common complication of diabetes. Reducing overall caloric intake and increasing the consumption of healthy foods improves health in general.
Frequent exercise: The addition of a regular exercise regimen is equally important because exercise aids in weight loss, which is a vital part of managing diabetes.
If your child is diagnosed with type 2 diabetes, a doctor will usually prescribe these additional measures:
Medication: Besides lifestyle changes, children and teens with type 2 diabetes are often given anti-hyperglycemic drugs, taken by mouth, or insulin to reduce blood sugar levels. Consistency in taking prescribed medications is extremely important for keeping the disease in check.
Blood Sugar Monitoring: Parents, along with their children, should monitor blood sugar levels multiple times per day by pricking a fingertip with a lancet. A drop of the blood is then placed on a test strip and put into a meter for reading. The resulting numbers determine if an adjustment in medication is needed.
Regular Check-Ups: In addition to frequent blood sugar monitoring, children and teens should also have regularly scheduled doctor appointments—usually four times a year. Regular dental and eye check-ups are also important to provide early detection of any complications.
How can I best help my child who has type 2 diabetes?
Abundant support exists for parents who are helping their children adapt to living with type 2 diabetes. Beginning with the diagnosis, the child or teen’s physician will be the first to offer education in monitoring, medication, and management of the disease. Additional help may come from other medical professionals, such as a pediatric endocrinologist, from dieticians, and from support groups.
Parents should understand that the realities of being diagnosed with type 2 diabetes may be difficult for children and teens to accept. Emotional responses of anger, fear, and lack of cooperation are common; however, empathetic listening and supportive education can help with adjustment for both parents and children. Seeking support for the patient and the parent can be reassuring for both.