The Scenic City is teaming with outdoor activities and spring is one of the best times to get out and enjoy them. Unfortunately, it is also one of the worst times of the year for seasonal allergies in the Tennessee Valley. Just last year, The Asthma and Allergy Foundation ranked Chattanooga No. 3 on its list of the 10 worst cities for spring allergies in the United States. Does this mean that outdoor enthusiasts with seasonal allergies need to stay indoors from March through May? Absolutely not. A little common sense and some help from one of Chattanooga’s many board-certified allergists can help manage the sniffles and itching that accompany the warm weather of this beautiful season.
By Julianne Hale
Full PDF here.
The problem with pollen
“The medical literature reveals that up to 50% of the general population has some form of allergy, whether it’s to pollen, mold, food, stinging insects, etc.,” says Dr. Susan Raschal, a board-certified allergist with Covenant Allergy and Asthma Care. “Around 20-30% of these allergies are seasonal.”



Allergist, Convenant Allergy and Asthma Care
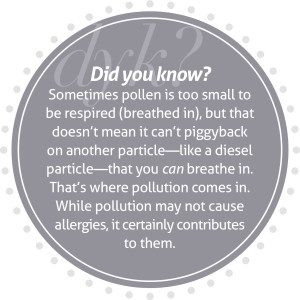
With the advent of spring comes tree pollen, perhaps the most problematic allergen of the whole year in Chattanooga. Dr. Raschal says the five most common tree pollens affecting Chattanoogans are hickory, maple, oak, sweet gum, and hackberry. Tiny and lightweight, these particles can be carried for miles on the fresh spring winds.
Dr. Robert Younger, a board-certified allergist with The Allergy and Asthma Group, explains, “You don’t have to look very far to see a forest here and tree pollens are huge in our area with all of the hickory and oaks. A severe pollen count is 100 per cubic meter and the pollen count in the Scenic City routinely exceeds 3,000 and has hit record counts in the past between 8,000 and 10,000.”
Spring allergies can begin as early as late February and typically last until May. The extent and duration depends on when the trees begin to turn green and generate pollen. Grass pollen takes over during the summer months, followed by leaves during fall.
If you’re one of the 20 to 30% of the population with seasonal allergies, your body responds by sneezing, itching, coughing and a general feeling of misery from the neck up.
Dr. Marc Cromie, a board-certified allergist at the Chattanooga Allergy Clinic, explains what happens in the body: “In seasonal allergies, the immune system overreacts to something that is typically benign. We cannot avoid pollen and our immune system is trying to protect itself and recognizes the pollen as a foreign body, causing IgE (Immunoglobin E, a type of antibody produced by the immune system) to be released, which starts an allergen cascade leading to the release of histamine. This release causes the typical symptoms of allergies—sneezing, coughing and itching.”



Allergist, Chattanooga Allergy Clinic
Treating mild to moderate allergies
If you experience mild or moderate symptoms due to seasonal allergies, your first line of defense is to avoid them. This means paying close attention to the pollen count and altering plans when the pollen is high as well as steering clear of common irritants such as cigarette smoke, perfume and pollutants.
It also means ridding your home of pollen and other allergens. Seal off the house by closing the windows during high pollen times and keeping the doors shut. Wash pets regularly to avoid the transfer of pollen from their fur to your home, use air purifiers to remove irritants from the air, and avoid synthetic fabrics which can create static electricity that attracts pollen to your clothing.
In addition, people with mild to moderate allergy symptoms—like sneezing, coughing and itchy eyes and nose—can use second generation, non-sedating antihistamines to alleviate symptoms. These medications are widely available over-the-counter. They include Zyrtec, Allegra, Claritin, and Clarinex.
If these don’t work, you may need to go with something stronger. “If your nasal congestion persists and you experience blockage or stuffiness in the nose and the antihistamines are not effective, a nasal cortisone spray, sold under the brand name Nasacort, is now available for over-the-counter use,” explains Dr. Younger.



Allergist, The Allergy and Asthma Group
Nasacort is big news in the allergy community, offering safe relief for allergy sufferers without a prescription. “Nasacort is an intranasal steroid and intranasal steroids are the single most effective medication for the treatment of mild to moderate allergies. It’s a great medication,” says Dr. Raschal. “In order to experience maximum results, patients will need to take the drug for 7 to 14 days so that it will be optimized by the body.”
Unlike well-known nasal sprays, Nasacort is not a decongestant and does not have the associated dependency risk and negative side effects that these drugs have. “Nasal steroids are very safe,” assures Dr. Raschal. “The most common side effect is a bloody nose and, in most cases, that can be prevented by pointing the spray away from the midline of the nose.”
Help for serious seasonal allergies
One common misconception for seasonal allergy sufferers is that there is no real relief. Many assume that allergy testing is for people with perennial allergies and not people who go through more tissues during the spring months than the rest of the year combined. Dr. Younger elaborates, “It is remarkable to me how much misery people with seasonal allergies will put up with to get through the spring,” he says. “It’s not necessary. We [allergists] can do so much to help alleviate the symptoms of seasonal allergies.”
If you have avoided being outdoors on high pollen count days, taken non-sedating antihistamines, and used Nasacort for two weeks without ample relief, it’s probably time to make an appointment with your local board-certified allergist.
Knowledge is power and an allergist will use a combination of an examination and health history to gather information about your case, but the most powerful tool in the allergist’s toolbox is the allergy test. The first part of this simple test involves a scratch test, in which the surface of the skin is lightly scratched with several plastic, toothpick-like points to introduce a variety of common allergens. The skin’s reaction to these scratches lets the allergist know whether or not the patient has an allergy to each substance and the severity of that allergy. The second part of the test involves an intradermal introduction of allergens just under the skin through a small injection. This allows the doctors to gain a comprehensive understanding of each patient’s particular allergies so that they can create a custom treatment plan to relieve their allergy symptoms.
Sometimes, an allergist uses information gathered from an allergy test to create immunotherapy, commonly called allergy shots. “Immunotherapy changes the way the immune system reacts by teaching it to tolerate pollen,” Dr. Cromie explains. “Allergy shots are purified extracts of pollen, dander, and other allergens that are tailor-made based on what each person is allergic to. By injecting a small amount and gradually increasing the dose, the immune system begins to see these allergens in the blood and change the way it reacts to them. The immune system learns that pollen and other allergens are no longer dangerous and does not respond with an allergic reaction. The shots are incredibly effective, with an 85 to 90% success rate.”
But allergy shots aren’t for everyone. According to Dr. Raschal, testing positive for allergies doesn’t necessarily mean you need immunotherapy. “Allergy testing is important because it can confirm suspicion, but it doesn’t always mean a person needs allergy shots,” she says. “I tell patients to maintain a diary of their symptoms as well as triggers that can cause symptoms like irritants, air pollutants, temperature changes, pressure changes, and inhalants like mold and pollen. If symptoms correspond with weather or seasonal changes, but are unaffected by high pollen, a patient might not need allergen immunotherapy despite high-grade reactivity revealed by the skin tests.”
Looking to the future, researchers and pharmaceutical companies continue to make great strides in developing new treatments that may provide an alternative to shots. For example, in recent years, sublingual immunotherapy (SLIT), a treatment in which an allergist gives a patient small doses of an allergen under the tongue to boost tolerance, has begun to gain the attention of allergists in the U.S. However, while it is gaining in interest, it has not yet been approved by the FDA. Additionally, American pharmaceutical companies are beginning to develop allergy immunotherapy in the form of tablets. Merck & Co. has already developed a tablet for the treatment of allergic rhinitis, and The American College of Allergy, Asthma and Immunology reports the likely approval of a tablet for ragweed before the end of 2014 and another for dust mites in early 2015. However, it should be noted that at this time, these tablets are designed to treat only a single allergy (for example, grass as opposed to a variety of allergies). Additionally, they have not yet been shown to be able to change the response of the immune system and prevent the development of asthma – another advantage of allergy shots.
There is no reason to suffer with seasonal allergies when so many effective treatments are right at our fingertips. If you have seasonal allergies, use common sense when it comes to outdoor and indoor exposure and take the suggested over-the-counter medicines to help alleviate symptoms. If that doesn’t work, make an appointment with an allergist and let them help you enjoy the spring without the itching, sneezing and coughing. You’ll be glad you did.
See Related Articles