With more than 60 million cases reported each month, acid reflux and gastroesophageal reflux disease, also referred to as GERD, are some of the most common digestive diseases in the U.S. Journey along to learn the signs, symptoms, and treatment options for these prevalent but preventable conditions.
What Is Acid Reflux?
According to medical terminology, it’s gastroesophageal reflux or GER, but you’ve heard it called acid reflux. This condition is caused by an issue with a small valve muscle at the entrance to your stomach called the lower esophageal sphincter, or LES.


When your LES opens too often or doesn’t come to a complete close after you’ve eaten, stomach acid can wash upward into your esophagus, which causes heartburn.
When you have acid reflux more than twice a week for two to three weeks, it’s considered chronic and tends to be referred to as gastroesophageal reflux disease, or GERD. According to Dr. Richard Pigg, a family medicine physician with CHI Memorial Primary Care and Sports Medicine Associates, “Acid reflux becomes GERD when it causes bothersome symptoms or injury to the esophagus.”
While heartburn is often the primary symptom of the disease, not all adults with GERD have heartburn.
Dr. Robert Bosshardt, a gastroenterologist with Galen Medical Group, explains, “Heartburn and regurgitation are the hallmark symptoms, but you may also experience coughing, non-cardiac chest pain, chronic laryngitis, asthma, and difficulty swallowing.”
There isn’t a single cause of acid reflux and GERD, but there are many potential factors. “One of the biggest risk factors for GERD is obesity,” says Dr. Bosshardt. “Age can also play a role, and certain medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDS) like ibuprofen, can worsen reflux.”
Another common risk factor is a hiatal hernia. This is when a portion of your stomach slides up through an opening in your diaphragm called the hiatus, making it easier for food and acid to travel back into the esophagus. Dr. Eston Wenger, a surgeon with Surgical Associates of Cleveland, explains, “Hiatal hernias can be caused by anything that puts pressure on your abdomen, whether it’s pregnancy, obesity, heavy lifting, or even coughing.”
Cigarette smoke is another major risk factor for GERD. Nicotine causes your LES muscles to relax, allowing stomach acid to leak into your esophagus. Progesterone, a hormone that spikes during pregnancy, can cause the LES to loosen as well, making heartburn a common but unpleasant side effect of pregnancy.
What Can It Lead to?
If left untreated, GERD can lead to permanent esophageal damage. Dr. Wenger explains, “Barrett’s esophagus is a condition in which your body replaces the tissue that lines your esophagus with tissue resembling the lining of your intestines” – a protective measure against repeated acidic abuse. While only a small portion of those plagued by chronic GERD will develop Barrett’s esophagus, it can lead to esophageal cancer.
Prolonged, untreated GERD can also cause scar tissue to form in the esophagus. “The scar tissue narrows the pathway, making it much more difficult, and often painful, to swallow,” says Dr. Pigg.
Other complications from repetitive acid reflux include tooth decay, severe esophageal irritation presenting itself as esophageal ulcers, and bleeding. It’s also possible for stomach acid to make its way into your lungs, causing respiratory issues like pneumonia, asthma, or laryngitis.
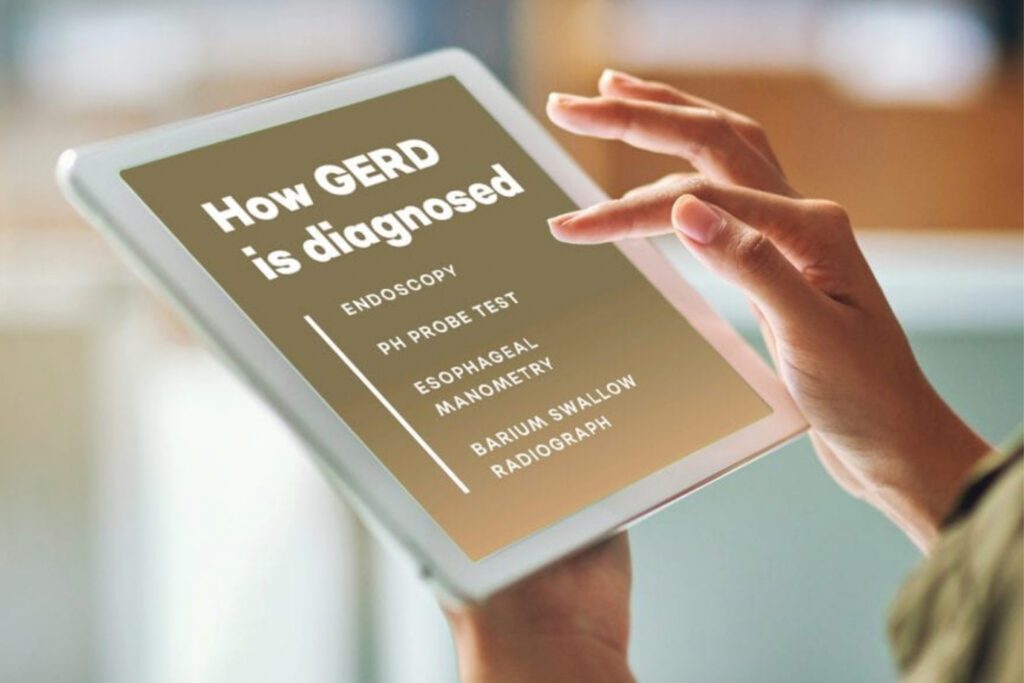
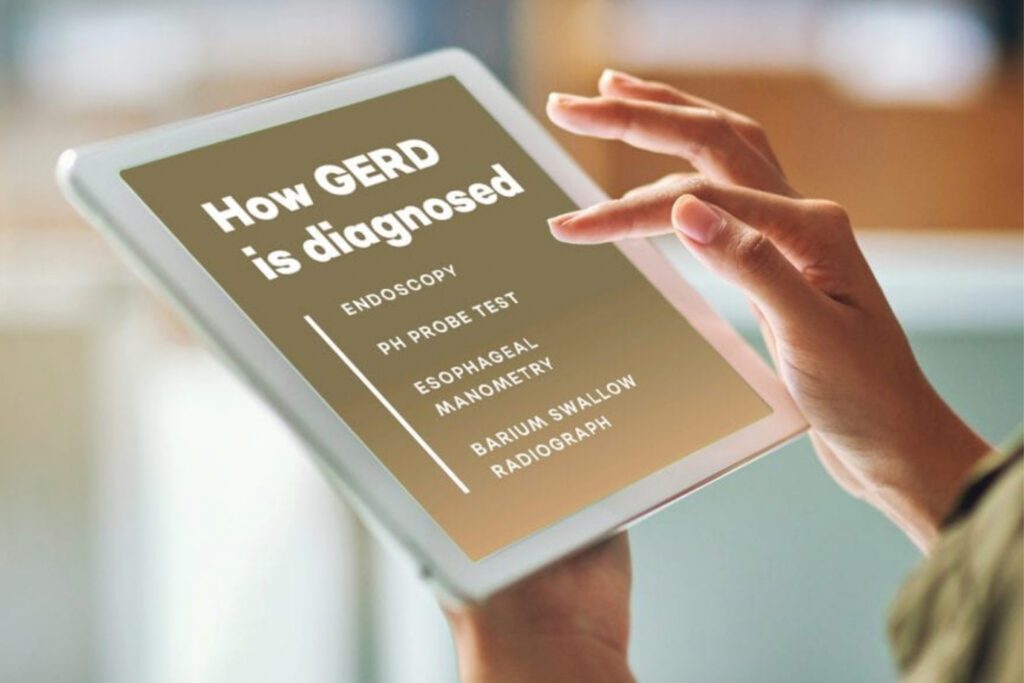
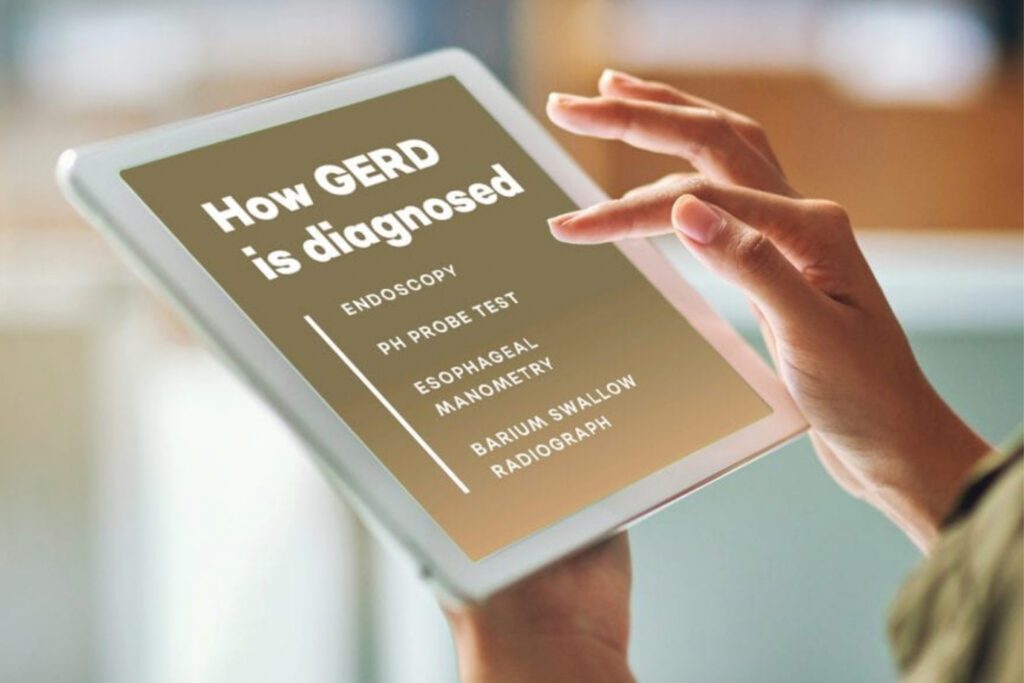
How Is It Diagnosed?
In patients with classic symptoms such as heartburn and regurgitation, acid reflux and GERD can be diagnosed clinically."
Dr. Pigg
“In patients with classic symptoms such as heartburn and regurgitation, acid reflux and GERD can be diagnosed clinically,” explains Dr. Pigg. But to confirm the diagnosis or to check for complications, tests may be necessary.
One of those tests is an endoscopy, where your gastroenterologist or surgeon will insert a small, flexible tube with a camera and a light at the end of it down your esophagus and into your stomach. The endoscope transmits a video to a monitor, allowing your doctor to inspect your GI tract for evidence of prolonged damage.
Another test is a pH probe. For a pH probe, your doctor will guide a thin probe through your nose or mouth to the end of your esophagus. This probe connects to a device that measures when and how much acid enters the esophagus while you go about your routine dietary and sleep habits for 24 to 48 hours.
In an esophageal manometry, your doctor will pass a thin tube through your nose into your stomach.
When you swallow, the doctor pulls the tube slowly back up your esophagus as it measures and records the muscle contractions throughout your esophagus.
Another method to diagnose GERD is through a barium swallow radiograph. This is similar to an X-ray, but first you’ll drink a barium solution to highlight your esophagus and GI tract. This method can detect structural issues with your esophagus, but since those issues are only present in one third of people diagnosed with GERD, a barium study may not be conclusive for diagnosis.
Cooling the Burn
Acid reflux and GERD symptoms are typically managed with a step-up approach, beginning with lifestyle changes that include:
Avoiding trigger foods.
Certain foods can trigger or worsen acid reflux. Try to avoid spicy foods, fried foods, fatty red meat, citrus fruits, mint, onions, tomatoes, caffeine, and chocolate.
Quitting smoking.
In addition to relaxing the LES, studies show smoking reduces the amount of saliva your body produces, which in turn limits your body’s ability to wash acid out of your esophagus.
Evaluating your sleep position.
Sleeping with your stomach below your esophagus helps gravity do its job and keeps your stomach contents where they’re supposed to be. Doctors recommend raising the head of your bed six to eight inches using blocks or even books.
Eating smaller meals, more frequently.
A full stomach is more likely to put pressure on your LES, so eat smaller meals more often to keep yourself full without the reflux.
Skipping the alcohol.
As with nicotine, alcohol causes your LES to relax. Studies also show it can cause esophageal spasms, and the acidity of alcohol can exacerbate heartburn. If you are planning to drink, try to limit your intake and cut yourself off several hours before bed.
Upping your exercise routine.
Studies say obese people are almost three times more likely to have acid reflux than those maintaining a healthy weight. Extra poundage can put pressure on your stomach, which forces acid into your esophagus.
Drinking more water.
Water neutralizes the pH of gastric acid within a minute. In essence, every time you take a drink of water, you temporarily dilute your stomach acid.
Taking an antacid.
Your doctor may recommend over-the-counter antacids or H2 blockers, which decrease stomach acid production. In more severe cases, your doctor may prescribe a proton pump inhibitor. As these medications have been linked to a number of side effects, they’re not typically used as a first line of defense.
“If you experience acid reflux several times a week, are 50 or older and have had reflux for an extended period of time, or have a family history of esophageal cancer, make an appointment with your doctor,” advises Dr. Bosshardt. In most cases, lifestyle changes, medications, or even a safe laparoscopic surgery can relieve symptoms. “Whatever the treatment may be,” Dr. Wenger says, “the goal is to improve your quality of life.”



Dr. Eston K. Wenger
Surgeon, Surgical Associates of Cleveland



Dr. Richard Pigg
Family Medicine Physician, CHI Memorial Primary Care and Sports Medicine Associates



Dr. C. Robert Bosshardt
Gastroenterologist, Galen Medical Group

