Colon cancer is the third most commonly diagnosed cancer and the second leading cause of cancer death in men and women combined. But with screening, it’s preventable, treatable, and beatable.
By Rashad J. Gober



Assistant Professor of Clinical Medicine, University of Tennessee College of Medicine Chattanooga, Gastroenterologist, Academic Gastroenterology, Erlanger Health System
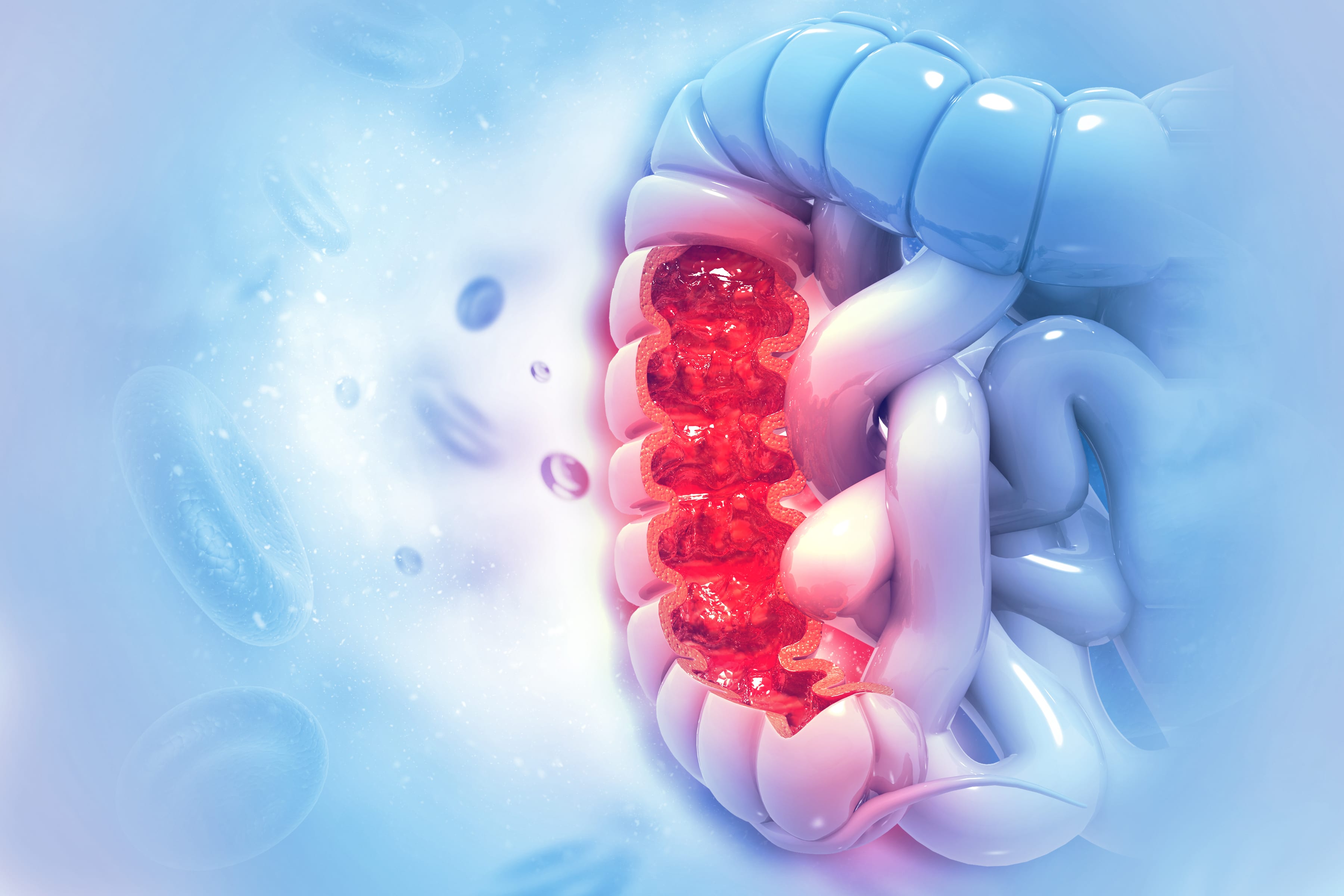
All About Polyps
A colon polyp is a small cluster of cells that forms on the lining of the colon. Most of the time, cells grow and divide in a very systematic fashio. However, sometimes, mutations in certain genes can sometimes cause cells to continue to divide unnecessarily and form a tissue growth. Colon polyps are actually very common in adults, and while not all polyps are dangerous, almost all colon cancers begin this way. “Over time, a polyp can grow larger and develop pre-cancerous changes that eventually develop into cancer,” explains Dr. Arslan Kahloon, a gastroenterologist with Erlanger Health System.
What Might Put You at Risk
Age is the biggest risk factor for developing colon polyps – most people with colon polyps are age 50 or older. Also, the incidence rate of colon cancer is highest in African-Americans, so doctors often recommend earlier screening. Other risk factors include poorly controlled type 2 diabetes, inflammatory intestinal conditions (e.g. Crohn’s disease), obesity, smoking, and heavy alcohol use.
When Colon Cancer is Inherited
Family history also plays a role in determining your risk of developing colon polyps. Though most cases are sporadic (non-inherited), around 5% of individuals with colon cancer have a hereditary form caused by abnormal genes passed down from a parent.



Clinical Gastrointestinal Pathologist, Diagnostic Pathology Services, CHI Memorial
According to Dr. Thomas Brien, a gastrointestinal pathologist with CHI Memorial, these hereditary forms of cancer tend to occur at an earlier age, and there is a very high likelihood of inheriting these genes from an affected parent. “If a parent has a gene mutation, then each of his or her children has a 50% risk of receiving it,” he says.
Scientists have identified two common forms of hereditary colon cancer influenced by mutations on specific genes. One is familial adenomatous polyposis (FAP), which doctors have linked to the APC gene on human chromosome 5. According to the National Human Genome Research Institute, those who inherit mutations in this gene have an almost 100% chance of developing colon cancer by age 40.
Hereditary nonpolyposis colon cancer (HNPCC), or Lynch syndrome, is the other common form. Those with an HNPCC gene mutation have around an 80% likelihood of developing colon cancer during their lifetime. “It’s very important to find out if you have Lynch syndrome, because colon cancer is not the only type of cancer it puts you at risk for,” says Dr. Brien. “It also puts you at high risk of uterine (endometrial) cancer.”
Red flags for hereditary forms of colon cancer include having multiple family members who have been diagnosed with it (for example both a parent and a grandparent or a parent and an uncle or aunt) or a family member who has been diagnosed at a younger age (<50). “If any of these things are true for you, it would be beneficial to consider genetic testing,” says Dr. Brien. “Don’t ignore your family history. If you don’t know it, ask your relatives.”



How do I know if I have colon cancer?
In most cases, colon cancer won’t cause symptoms until it has advanced and spread, so everyone should be tested before developing symptoms. “Small polyps usually don’t cause any symptoms at all,” Dr. Kahloon explains.



Colorectal Surgeon, Parkridge Health System
The good news is colon cancer is very easy to treat if polyps are discovered early. “It usually takes five to 10 years for a polyp to develop into cancer, but there are some forms that are more aggressive and go faster,” says Dr. Shauna Lorenzo-Rivero, a colorectal surgeon with Parkridge Health System. “But with screening, colon cancer is preventable, treatable, and beatable.”
Some signs and symptoms of colon cancer in a later stage include unexplained changes in your bowel habits (i.e. diarrhea, constipation, or change in stool consistency), blood or mucus in your stool, crampy abdominal pain, and unexplained weight loss.
If you have any of these symptoms, it is important to consult your doctor as soon as possible. However, don’t let your experience automatically lead you to the worst-case scenario. Often something that isn’t cancer – like hemorrhoids, an infection, or irritable bowel syndrome – is the culprit behind these symptoms.
Getting Screened
As mentioned above, screening for colon cancer is so important because if your doctor finds cancerous polyps when they are confined to the colon, they are almost always treatable. Modern medical guidelines recommend that those at normal or average risk for colon cancer get their first screening colonoscopy at age 50.
In a colonoscopy, a doctor uses a long, lighted tube to examine the inside of the rectum and the entire colon. The day before this test, you may be required to adhere to a clear liquid diet and use laxatives to clean out your colon. You will also need to be sedated and the whole procedure takes about 30 minutes to an hour.
The benefits of the colonoscopy are that the doctor can view your entire colon and rectum and remove anything potentially dangerous right away. “Benign or precancerous polyps can be removed by a gastroenterologist during the procedure, completely preventing cancer from developing down the road,” says Dr. Kahloon.
Dr. Lorenzo-Rivero explains that for those at average risk for colon cancer, this test should be performed every 10 years. However, those at high risk will need it earlier and more frequently. “If you are high risk, meaning you have had a first-degree relative with polyps, you should get your first colonoscopy at the age of 40 or 10 years before the youngest person in your family was diagnosed. From there, you should continue to get a colonoscopy every five years. Those who have had polyps before will also need one every five years.”
Another form of colon cancer screening is the virtual colonoscopy, or CT colonography. For this test, a small catheter is inserted into the rectum to fill your colon with air or carbon dioxide. You don’t have to be sedated for a virtual colonoscopy and it only takes about 15 minutes. However, if polyps are discovered during this test, a colonoscopy will need to be performed in order to remove them.
A third way to screen for colon cancer is the fecal occult blood test (FOBT), which looks for hidden blood in the stool. If blood is found in the stool, then a colonoscopy will need to be done.
The kind of test you choose and the frequency of your testing will depend upon your risk factors. Talk with your doctor about which test is right for you and how often you should be screened. Whichever screening method you choose, be sure to stick to the screening schedule because early detection is crucial when dealing with colon cancer.
Don’t wait!
If you’re 50 years of age or older or have significant risk factors for developing colon cancer, talk to your doctor about getting screened today. “The main message I would like to send to be people is: get your colonoscopy now,” says Dr. Lorenzo-Rivero. “If you are over 50 and haven’t gotten one, please do it, not just for yourself, but the people who love you.”
For more statistical information about colon cancer, visit cancer.org. For more information about colon cancer prevention and screening, visit mdanderson.org.



See Related Articles