What’s The Connection Between Weight Gain and Type 2 Diabetes?
The prevalence of those who are overweight or obese in the United States has been on the rise for decades. The Centers for Disease Control (CDC) calls obesity an “epidemic” in our nation, and it’s one of the most serious and costly medical conditions. According to Dr. Anders Petersen, a board-certified family practitioner with HealthWorks, the obesity epidemic has been propelled by the “[move] toward a more sedentary lifestyle and the availability of fast food and processed food.” But more than needing to go up a pant size, what are the costs for so many Americans who watch in trepidation as the numbers on the scale continue to rise?
The Costs of Extra Weight
As for the cost in dollars, the CDC explains that obesity costs the U.S. healthcare system almost $173 billion a year. Additionally, according to the National Library of Medicine, a study was conducted that found the annual medical care expenditures of adults with obesity (defined as anyone with a BMI greater than or equal to 30kg/m²) were double those of adults who were normal weight.
Besides being hard on finances, obesity can also come with other costs. Namely, serious medical conditions. From heart disease, to stroke, to certain kinds of cancer, it’s no wonder the CDC sees obesity as a serious condition.
Of particular concern is type 2 diabetes. Being overweight or obese is, by far, the number one risk factor for the condition. The American Society for Metabolic and Bariatric Surgery reports that 90% of people with type 2 diabetes are overweight or obese.

Diabetes also damages small blood vessels throughout the body, and it can lead to blindness, kidney failure, amputation, and premature death. According to the Mayo Clinic, those with diabetes also have a higher risk of developing depression.
Of course, adults aren’t the only ones affected by the epidemic. The number of overweight or obese children is rising dramatically. According to the World Health Organization, the prevalence of overweight in children (ages 5 to 19) has risen from 8% in 1990 to 20% in 2022.
What is Diabetes? The Basics
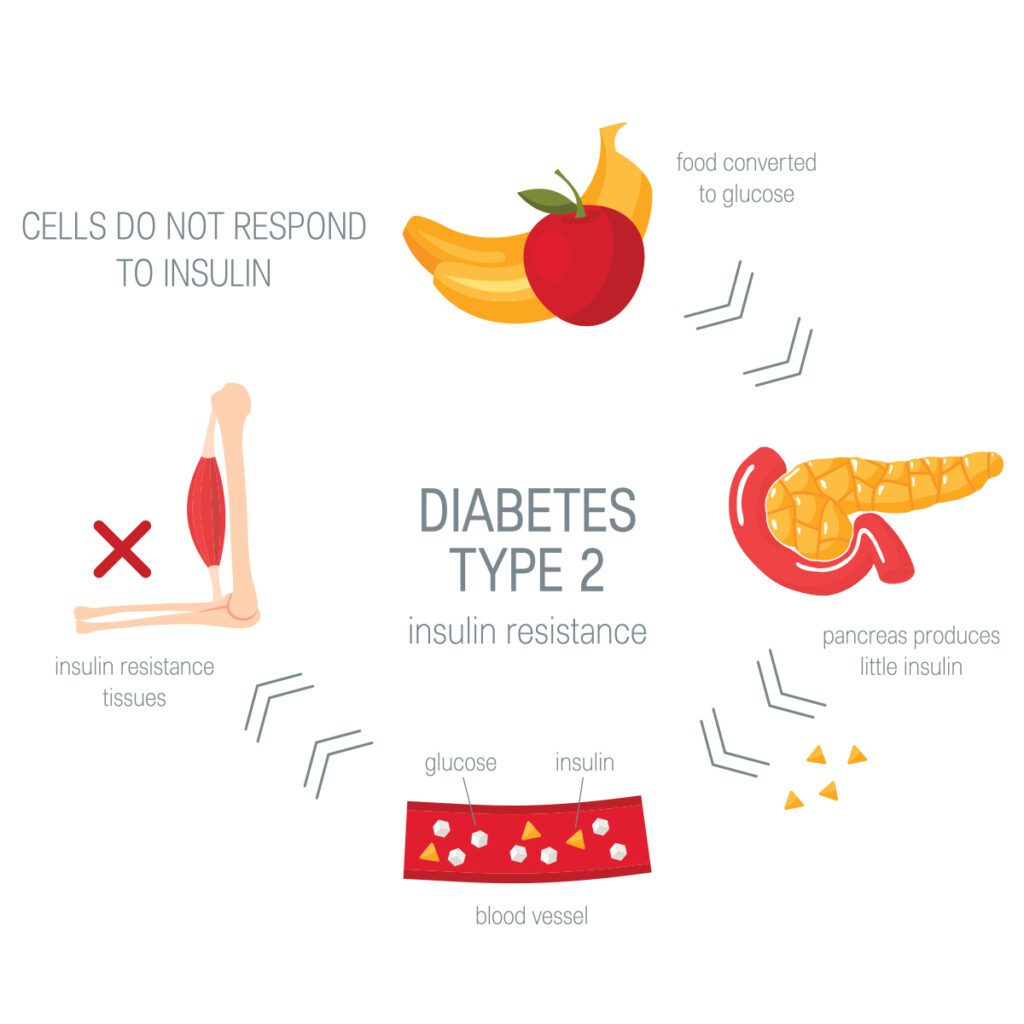
Diabetes affects how the body uses and processes blood sugar, or blood glucose. Glucose is a source of fuel used by the body. The pancreas makes insulin, which, in turn, moves glucose from the bloodstream into muscle, fat, and liver cells where it is used as fuel. With diabetes, the body is limited in how well it can process glucose from the bloodstream into usable fuel. Either the pancreas does not make enough insulin, the body does not respond to insulin normally, or there is a combination of both.
People with type 1 diabetes have high glucose levels because their pancreas can no longer make insulin. By definition, these diabetics must eventually take insulin shots to get their diabetes under control. Type 1 diabetes is commonly seen in children where it is diagnosed as a lifelong disease. According to Leslie Roberts, a dietitian with the Hamilton Diabetes and Nutrition Center at Hamilton Medical Center, patients with type 1 are “usually younger and typically thinner.” Additionally, there is usually a genetic link to their diabetes.
Yet, while type 1 diabetes is more commonly seen in adolescents, Roberts explains that there has been an increase in the amount of adults diagnosed as well—this has led to the extinction of the term “juvenile diabetes.” Like adolescents with type 1 diabetes, these adults tend to have a thin physique and a genetic link to their diabetes.
Type 2 diabetes is far more common, making up 90-95% of cases. Type 2 diabetics can still make their own insulin, but their bodies’ cells don’t respond well to it—a situation called insulin resistance. Roberts explains that nearly all of the patients she sees with type 2 diabetes are “overweight and typically live a sedentary lifestyle.” However, there are cases where type 2 diabetes has developed in a patient of a normal weight.
Weight, insulin resistance, and Type 2 Diabetes: What’s the Link?
Let’s discuss why excess weight increases the risk of type 2 diabetes. Many researchers note that fat cells— especially those in the belly, where people tend to carry extra pounds—secrete hormones and other chemical signals. Some of these substances can trigger inflammation, which interferes with insulin receptors on cells, leading to insulin resistance and high blood sugar.
If blood sugar levels stay high, your pancreas has to continue pumping out enormous amounts of insulin to force the uptake of glucose in your cells. This only exasperates the issue because repeated surges of insulin can strip your cells’ insulin receptors even more—cells overwhelmed by surplus insulin will protect themselves by continuing to reduce the number of their insulin receptor sites.
Thus, the vicious cycle begins: the more insulin your body has to produce to keep blood sugar down, the more insulin resistant you become. Eventually, the pancreas can’t keep up, and you are left with chronic high blood sugar, also known as hyperglycemia. This is problematic for two reasons:
- While you may not have type 2 diabetes yet, you are well on the way with all of the stress that this resistance puts on your blood sugar control system. Essentially, your cells are starving for energy, even when plenty of glucose is available in the blood. If it goes on for long enough, the insulin-producing beta cells in the pancreas can “burn out.” If they die off entirely, you’ve got full blown diabetes.
- Over time, if high blood sugar levels go unchecked, your body will become used to storing the overabundance of glucose as fat. Thus, insulin resistance can potentially lead to even more weight gain.
Of course, the relationship between weight, insulin resistance, and type 2 diabetes is far more complex than this. While the idea that there is a connection between weight and insulin resistance is undisputed, scientists are still left with a “chicken and the egg question:” does excess body fat cause insulin resistance or is it the other way around?
Complicating the issue even more is the fact that many obese people are not insulin resistant, and not everyone who is insulin resistant is overweight. Some people have a genetic predisposition to insulin resistance; scientists have identified specific genes that make people more likely to develop the condition.
Type 2 Diabetes & Normal Weight
While those who are overweight or obese are far more likely to have type 2 diabetes, it’s not impossible for those of a normal weight to contract type 2 diabetes.
For these people, the disease can be even more dangerous than it is for someone who is overweight. Referred to as “the obesity paradox,” studies have shown the risk of death in patients with type 2 diabetes who are obese or overweight is lower than the risk of death in patients with type 2 diabetes who are of a normal weight.
Type 2 Diabetes & Normal Weight
If you think you might be in danger of being prediabetic or contracting type 2 diabetes, ask your health care provider about getting a fasting glucose test. Diabetes tends to start quietly and move slowly, often taking years before it is noticed. According to the CDC, around 98 million Americans have prediabetes, but more than 8 in 10 adults are unaware they have it.
The fasting glucose test measures your blood glucose level after you have gone without food for eight hours, so it’s usually done in the morning. A healthcare provider will take a sample of your blood, and then send it to a lab for analysis.
Your results will show how much glucose is present in your blood in milligrams (mg) per deciliter (dl). According to the Mayo Clinic, fasting glucose test results can be categorized as follows:

- Normal: below 100 mg/dl
- Prediabetic: 100 mg/dl to 125 mg/dl
- Diabetic: 125 mg/dl or higher, on two separate tests
According to the CDC, those who fall into the prediabetic range should understand that they are in serious danger of contracting diabetes within the next five years. However, with proper management and lifestyle changes, the condition is potentially reversible. According to the Mayo Clinic, one large study showed that individuals decreased their risk of developing diabetes by 60%, just by losing 7-10% of their body weight.
Taking Action
According to Dr. Petersen, one of the best things we can do is to educate people when it comes to weight gain and diabetes. “We need to know what’s going on in [our] bodies and how to change it,” he says. It’s important for patients to “take ownership of what they’re eating,” and to know that “even a small reduction in foods high in sugar and fat” can be of great benefit.
Americans who care about their weight and where their health is headed are far more likely to succeed in preventing the onset of diabetes. Diet and exercise are some of the best tools for warding off the development of diseases like diabetes.

Regular Exercise. Exercise can help you lose weight, and it can also help to lower your blood sugar by forcing your muscles to use the glucose in your bloodstream for fuel. This, in turn, can lower your body’s resistance to insulin by making your cells work harder to use up the available glucose. Exercise can also boost your number of insulin receptors.
Proper Diet. If you don’t watch your calories, the benefits of exercise will be limited. Plus, many studies have found that cutting calories can improve insulin sensitivity and reduce levels of circulating insulin (your body needs less insulin if it’s more sensitive to it).
But perhaps just as important as caloric intake are the kinds of foods you’re getting those calories from. Those who are at risk for diabetes may greatly benefit from a high-fiber, low-glycemic diet. Eating foods that keep blood sugar levels stable can be key to preventing or reversing insulin resistance. Fiber slows the speed at which your stomach empties after a meal, which also slows the rise in blood sugar that happens after you eat.
Bariatric Surgery
For many Americans, diet and exercise programs have not given them the results needed to manage and cope with their type 2 diabetes. In these cases, more extreme measures may be considered. One of these is bariatric surgery, which involves the removal of parts of the stomach and small intestines to induce weight loss.
Bariatric surgery may be considered a specific treatment for type 2 diabetes since morbidly obese people who’ve undergone gastric bypass (a type of bariatric surgery) usually see significant improvements in their blood sugar levels. In fact, according to the American College of Surgeons, 75% of patients who underwent a gastric bypass saw their type 2 diabetes stay in remission.
According to Dr. Sanborn, those eligible for bariatric surgery must have a BMI of at least 35, and most will have diabetes or another weight-related medical condition. But this alone is not enough; three additional criteria make a patient a good candidate for a bariatric surgery procedure. The first is motivation. “A motivated patient [is] probably the biggest key, because [bariatric surgery] is not something we do to you, it’s something we do with you. It’s not magic,” says Dr. Sanborn. The second criteria involves effort. “We want a patient to have tried diet and exercise and those aren’t working,” he says. Finally, Sanborn looks at patient expectations because “the surgery needs to fix more than just the numbers on the scale.”
Opting for a bariatric surgery procedure is a commitment that must be taken seriously. Those who are interested should speak with their doctor to determine if such treatment would be an overall beneficial choice. It takes motivation towards major lifestyle change for such procedures to be as effective as possible in treating obesity and type 2 diabetes.

While the outlook for obesity and type 2 diabetes may be grim, the potential for positive change in individuals is well within reach. With proper diet and exercise, we can significantly improve our health and reduce the chance of developing type 2 diabetes. Taking small steps every day to combat the disease can be as easy as a walk each day and enjoying a meal that is beneficial to your health. It’s the simple steps we take that, in the long run, can produce the most favorable outcome.
