Innovations in imaging and treatment techniques are improving outlooks for individuals with venous compression syndromes.
Understanding Venous Compression Syndromes
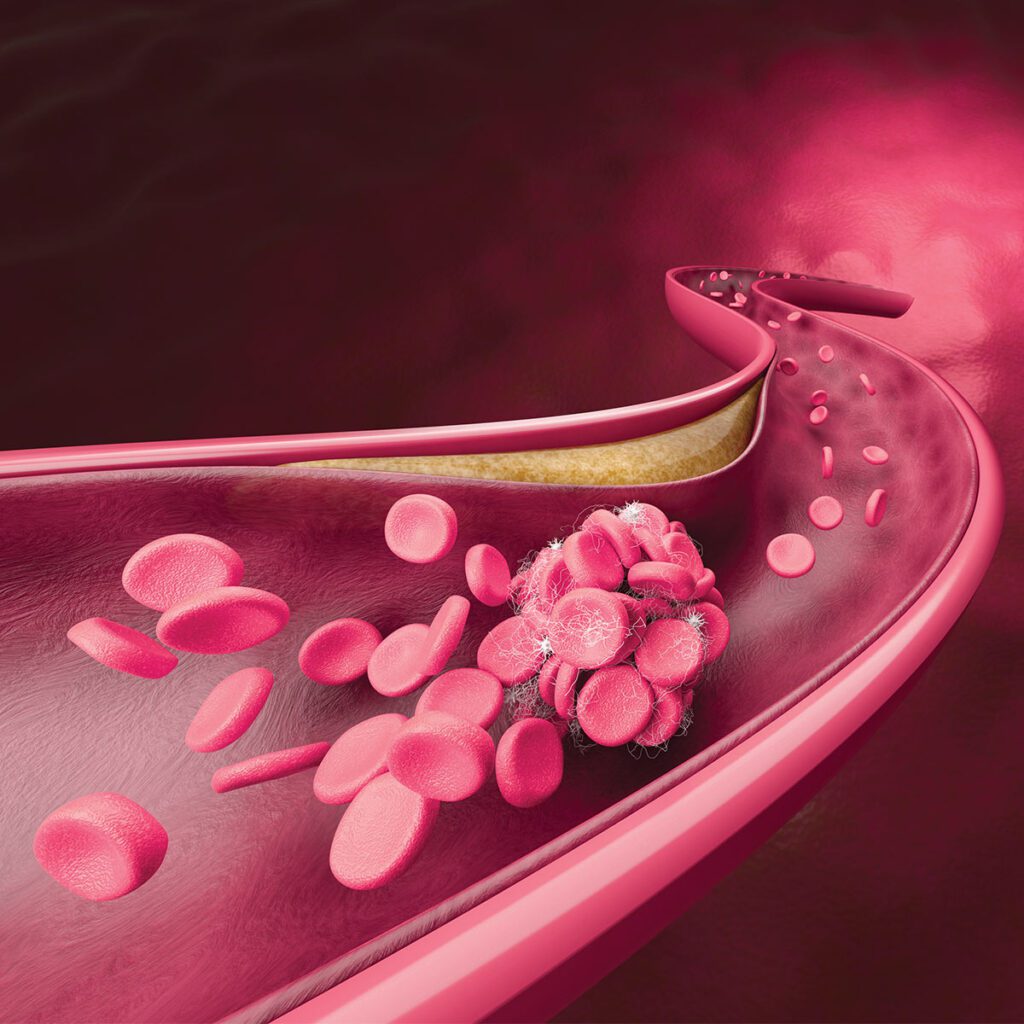
Venous compression syndromes occur when veins are compressed by surrounding structures, leading to impaired blood flow. Common types include May-Thurner Syndrome (iliac vein compression), Nutcracker Syndrome (renal vein compression), and Thoracic Outlet Syndrome (subclavian vein compression).
Causes and Symptoms
These conditions can be caused by anatomical variations or abnormalities or external factors like tumors, cysts, or scarring. Women are up to five times more likely to develop May-Thurner Syndrome, and genetic predisposition and family history also play a role in determining risk.
Symptoms include swelling, pain, or heaviness in the affected limb; varicose veins or venous ulcers; and blood clots, deep vein thrombosis (DVT), or chronic venous insufficiency (CVI).
Treatment Options
A clinical evaluation can assess and diagnose venous compression syndromes using innovative imaging techniques. These include:
- Duplex ultrasound, a non-invasive option that assesses blood flow and vein anatomy
- CT or MR venography, advanced imaging systems for detailed visualization of venous structures
- Intravascular ultrasound (IVUS), an invasive technique that provides real-time imaging inside the veins
Once diagnosed, there are many options available to treat these conditions. Conservation management can involve lifestyle modifications, compression stockings, and anticoagulation therapy. Endovascular treatments include angioplasty and stenting – minimally invasive procedures to open the compressed veins – and thrombolysis – medication to dissolve blood clots in cases of thrombosis. For some patients, surgical intervention may be recommended. Decompression surgery can remove the compressing structures and in severe cases, bypass surgery can create new pathways for blood flow.
Outlook
Long-term care includes monitoring with follow-up imaging and ongoing management of underlying conditions to prevent recurrence. Early diagnosis and intervention can prevent complications like CVI, recurrent DVTs, or pulmonary embolism and improve the quality of life with timely and appropriate treatment.
An Expert Weighs In
“Unexplained pain, pressure, and swelling in the upper and lower extremities is not normal and can be related to a problem with the circulation system. The venous side of the circulation brings blood back to the heart from the extremities. A blockage narrowing or constriction of the venous system reduces blood flow in the extremity and can cause severe symptoms. Vascular surgeons are the specialty that are trained to diagnose and treat arterial and venous conditions.”

Chris LeStar, MD, FACS, RVT
Vascular/Endovascular Surgeon, Vascular Institute of Chattanooga
Meet the Author

Rachel Studebaker, BA, English, Summa Cum Laude
Rachel Studebaker is a graduate of Lee University where she earned a Bachelor of Arts degree in English with a minor in advertising. While attending Lee, Rachel served as editor-in-chief and creative director for the school’s biannual publication Vindagua and was a member of Sigma Tau Delta English Honors Society. As managing editor for CMC Media & Marketing Group, she is responsible for the development and completion of 16 publications involving health, wellness, business, sports, and lifestyle articles published in print and online for HealthScope®, CityScope®, and Choose Chattanooga® magazines – premier publications serving S.E. Tennessee and North Georgia. Additionally, Rachel has led digital marketing initiatives for CMC Media & Marketing Group as well as the development of content for the introduction of Choose Huntsville™, Huntsville Resource & Relocation Guide™ for Huntsville, Alabama.
