If overlooked, this lethal skin cancer has deadly consequences. Here’s how you can protect yourself.
By Julianne Hale
WHAT IS MELANOMA, EXACTLY? Melanoma is the most serious type of skin cancer. It begins when something goes awry in the body’s pigment cells – called melanocytes – and they multiply rapidly, forming malignant tumors. Most melanomas form on the skin in a mole or a dark spot resembling a mole. But they can actually appear anywhere on the body where there is pigment – even the eyes.



Dr. C. Rodney Susong
WHY IT’S SO DANGEROUS: Melanoma is dangerous because of its ability to spread quickly to other parts of the body. Dr. Karin Covi, a dermatologist with the offices of Dr. C. Rodney Susong, explains, “Melanoma spreads to the skin immediately around the original lesion, but it can also be carried by the lymphatic system to the lymph nodes and through the bloodstream to other organs like the liver, brain, and lungs.” Sadly, melanoma rates have been rising in the U.S. for at least 30 years. The American Academy of Dermatology now estimates that 1 in 50 Americans will develop melanoma in their lifetime.
WHAT PUTS YOU AT RISK:
SKIN COLOR. This is the most significant risk factor of all. If you have fair skin, that means you have less pigment to protect you from damaging UV rays. People with lighter-colored hair, skin, and eyes are at the highest risk of developing melanoma. If your complexion is darker, you have a significantly lower risk; however, melanoma affects people of all skin colors.
UV EXPOSURE. If, like many of us, you spent your younger years at the tanning bed or local pool, you’ve been exposed to excessive ultraviolet (UV) light, which increases your risk of developing melanoma and other skin cancers. A history of severe sunburns also increases your risk.


MOLES. People who have an abundance of moles on their body, specifically 50 or more, face a higher risk for developing melanoma because moles are typically the starting point for the disease. Dr. Covi points out that a mole doesn’t have to be raised or warty to qualify as a mole. “A mole is anything pigmented on your body,” she says.
FAMILY HISTORY. If you have a family history of melanoma, you have a significantly higher risk of getting it yourself as some melanomas are caused by an inherited gene.


STAGING THE CANCER


Skin Cancer & Cosmetic
Dermatology Center
A skin biopsy is the only way to confirm a diagnosis of melanoma. Your physician will remove all or part of the suspicious growth and send it to a lab for analysis by a pathologist. The results, along with your doctor’s observations during the physical examination, will help determine the stage of the cancer.
Staging melanoma takes into account 1) the thickness of the cancer, 2) the depth of the cancer, and 3) how much the cancer has spread.
Dr. Eli Kim, a dermatologist with Skin Cancer & Cosmetic Dermatology Center, explains that it doesn’t take long to diagnose melanoma. “As dermatologists we see thousands of moles every month so we usually know right away if something looks abnormal,” he says. “If a mole has any warning signs at all, we will send it off to a pathologist and you will typically get the results within a week.”
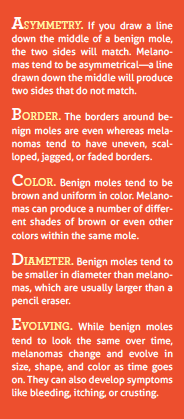
If you find yourself in an elevated risk category, you need to be on high alert when it comes to your skin. The Skin Cancer Foundation recommends a strategy developed by physicians to recognize the disease early. Called “The ABCDEs of Melanoma,” the acronym offers a simple reference guide for identifying key attributes of the disease. “Any of these alone increases your risk of melanoma, but the more you have, the higher your risk,” says Dr. Kim.
Yet while ABCDE is a useful acronym, be warned: melanomas sometime fall outside of its criteria. “I don’t know how often I hear the story, ‘It didn’t look typical for a melanoma’ and lo and behold it was,” says Dr. Mark Kelley, a surgical oncologist with CHI Memorial. “Melanoma doesn’t always look dark or alarming – many lesions don’t even have pigmentation. So if a skin lesion raises any question, see a dermatologist. It can make a huge difference.”
CHECKING YOUR SKIN:
May is Skin Cancer Awareness Month, so now is a great time to add a monthly skin check into your routine. “I encourage my patients to perform a self-exam every month,” says Dr. Covi. “If you know your own moles and freckles, you can immediately recognize anything that seems off – any ‘ugly duckling’ mole standing out from the rest.”
If you find a mole or spot that concerns you during your monthly self-screening, make an appointment with a dermatologist immediately. Otherwise, make sure to schedule a yearly skin check with a medical professional. “Everyone should have a professional total body skin examination on an annual basis, particularly those with a family history of melanoma, a history of abnormal moles, or lots of moles,” says Dr. Covi.


Dr. Kim agrees. “The American Academy of Dermatology recommends an annual skin check and that’s not just for people over 40,” he says. “It’s even more important for people if they have a family history of melanoma or a history of severe sunburn.”
Finally, if you have any personal history of melanoma, be extremely vigilant about follow-up appointments with your dermatologist or oncologist. Those at highest risk of melanoma are those who have already had it before – and had it spread. “The disease is known for behaving in a very unpredictable way,” says Dr. Kelley. “It has this ability to lie dormant for decades and come back later. That’s why ongoing surveillance – both for recurrence of the original melanoma and new ones – is so essential.”