Two of the most powerful diagnostic tools in use in medicine today are Magnetic Resonance Imaging (MRI) and Computed Tomography (CT).
Each of these, in its own right, is a relatively new technology, rising to prominence within the last 30-40 years and realizing continuous refinement along the way.
While both CT and MRI essentially provide enhanced images of body structures and/or tissues, they are distinctly different and are most effective in certain situations. During the diagnostic phase of treatment, a physician will assess symptoms and determine whether a need for CT or MRI is present. In a time-sensitive situation, particularly trauma, CT may be the initial approach. Then should a CT suggest the need, an MRI could follow; however, diagnoses related to soft tissue or organs may indicate the need for an MRI early.
How MRI Works
MRI uses high strength magnets to produce contrasting images of joints, muscles, blood vessels, and organs, including the heart. It provides very detailed images in virtually any plane. The first image produced by magnetic resonance was viewed in 1973. Four years later, the first MRI was performed on a human patient.
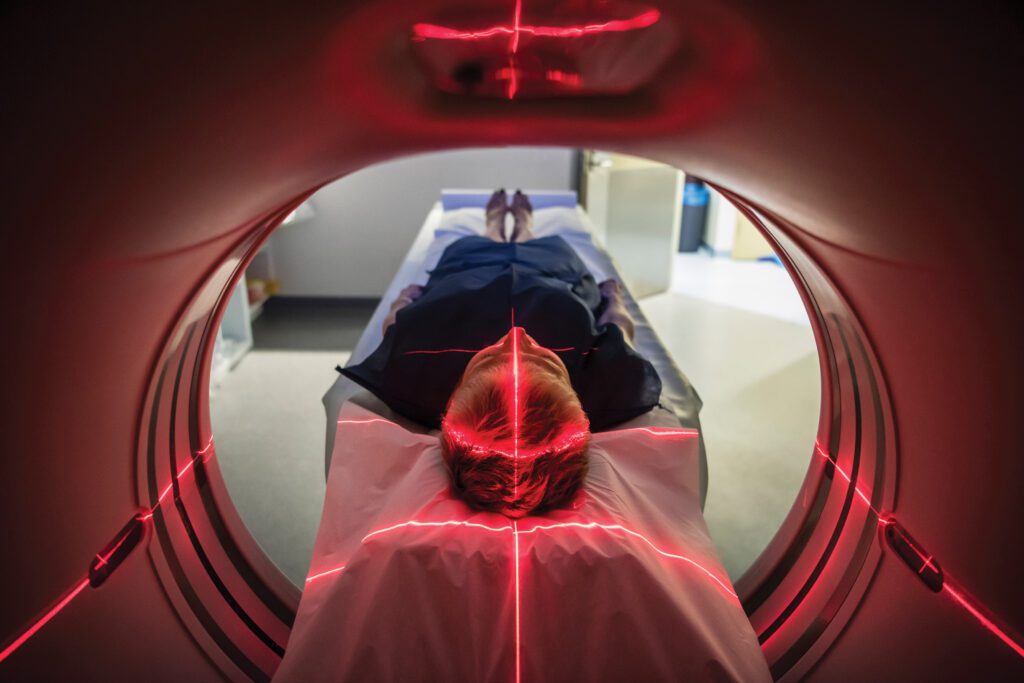
A patient undergoing an MRI is placed in a scanner, and the hydrogen nuclei, or protons, within the body’s cells naturally align with the main magnetic field produced in the scanner. During the scan itself, a second magnetic field, perpendicular to the first, is introduced and begins to oscillate at varied radio frequencies. The second magnetic field pushes the hydrogen nuclei out of their original alignment. As the scan proceeds, these protons return to their aligned positions and in doing so, emit a radio frequency . Protons in different tissues move at different speeds, and internal body structures are visible as this occurs.
If necessary, a contrast agent may be used to improve the quality of images which could reveal tumors, diseases of the blood vessels, or inflammation. One contraindication in the use of MRI involves patients with pacemakers.
How CT Works
Unlike MRI, CT traces its lineage to earlier radiation, or x-ray technology, which has been around for more than a century. CT generates two-dimensional images which can be reconstructed into three-dimensional views of an area, following a series of images taken around a specific axis of rotation. CT was first conceived in the 1930s, and it became medically viable in the early 1970s. CT often is used as a complement to or in lieu of conventional x-ray or ultrasound technology.
CT is sometimes utilized in diagnosing ailments of the heart, lungs, blood vessels, bones, and in detecting cancer. Although its use in a screening role is becoming more prevalent, some concerns remain as to cost/benefit. In other words, the “full body scan” may reveal an abnormality which triggers more testing and is ultimately of little concern while subjecting the patient to unnecessary radiation exposure and expense. When a patient is placed into a CT scanner, the x-ray source rotates around the area of the body to be scanned, and x-ray sensors are placed on the opposite side of the source. As the patient passes through the scanner, multiple images are created. Intravenous contrast agents can be used to produce CT images of the highest quality.
Use in Diagnoses
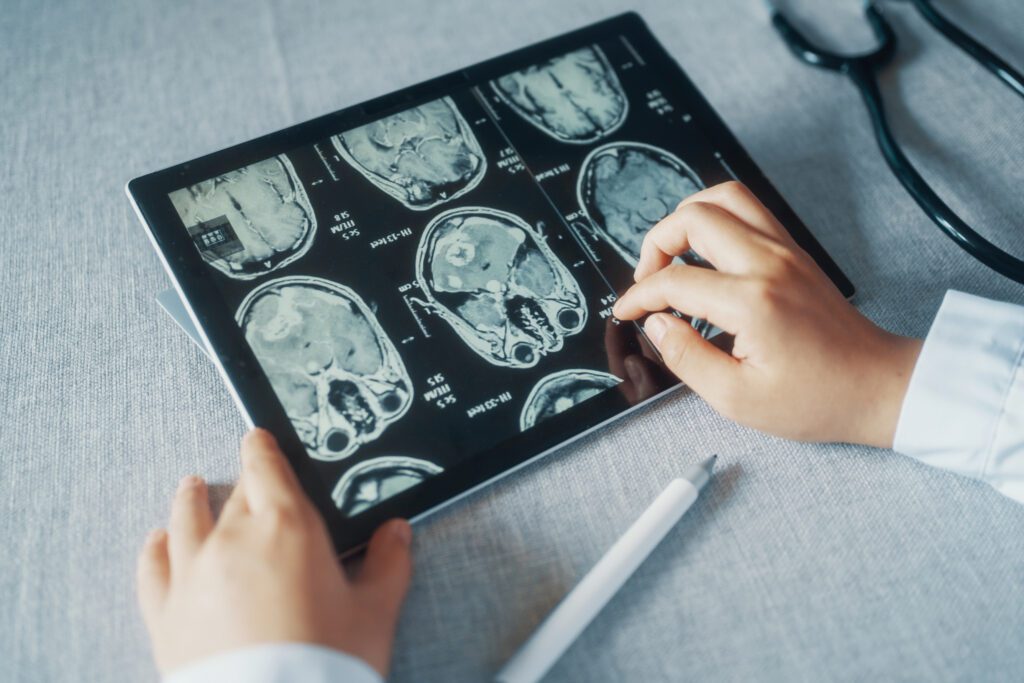
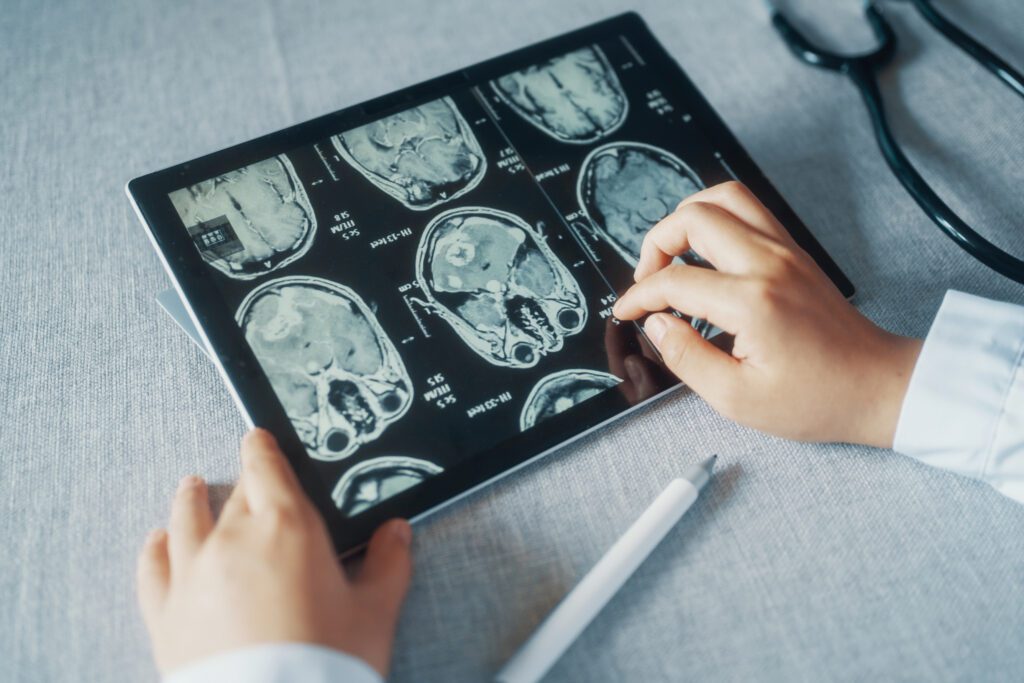
“Both of these imaging modalities have revolutionized the relative ease of diagnosis of many disease processes,” relates Dr. Scott Kemmerer of Tennessee Imaging and Vein Center. “They have enhanced a physician’s ability to pinpoint and accurately diagnose problems at an earlier stage of development. MRI is an imaging modality that uses a magnetic field and radio frequency energy to create a signal which generates images which can be used for diagnostic purposes. It is especially useful for soft tissues including the brain, and for joints and abdominal organs. More recently, biopsies are being performed, particularly in the breast, using MR guidance. CT scans use x-rays and multiple detectors to create images of the same body parts but can be obtained more quickly and are generally more widely available and slightly less expensive.
CT remains the work horse imaging tool for evaluation of the chest, abdomen and pelvis, while MRI has clear advantages in imaging the brain, musculoskeletal system and spine and has a significant problem-solving role in the abdomen and pelvis when CT is not adequate.”
In the ER
During emergency cases, particularly trauma, the CT is often the primary diagnostic tool used to determine the extent of a patient’s injuries.
“In any trauma situation that comes into an ER (emergency room), a patient will get a CT first, and then if there is a question on the CT that person would go to an MRI for further evaluation,” explains Dr. Steve Quarfordt of Chattanooga Imaging. “If a patient has a prominent fracture, you can see it on plain film, but then if there is greater concern, the evaluation could go to CT, and then if there may be more soft tissue involved, to an MRI. For example, a fracture of the vertebra may be determined by looking at a CT, but for information on what is occurring with the spinal cord, it may be necessary to do the MRI.”
Choosing the Most Appropriate Tool
One particular advantage of MRI in certain situations is that it does not expose the patient to radiation. “MRI is not x-ray and does not use ionizing radiation,” comments Dr. John Church of Dalton Imaging. “It is not dangerous to people in the strengths that we are using. So, particularly with children, you would prefer to use MRI rather than CT. Ionizing radiation can change the genetic makeup of a cell, causing mutations that can become problematic down the road. A lot of information is out right now about the overuse of x-rays with children, so in some things MRI is the first line for children. Ultrasound uses sound waves and is also good for children because it is not damaging.”
Generally, CT is acknowledged as the standard in rapid diagnosis and in the view of bone structure. CT scans may often be performed in a matter of seconds, while the MRI process is considerably lengthier.
“CT is good for trauma – and fast,” continues Dr. Church. “You can have a bunch of people in the room with a patient who is intubated, each of them doing their thing, but with MRI you can’t have a lot of wires and things going on during the scan. Also, about 40 percent of the patients who come into community hospitals with chest pain are having actual cardiac pain. The other 60 percent are having pain due to some other reason.”
“When people come into the ER with chest pain, the physician doesn’t immediately know if it is cardiac related, but there are three things that can kill you quickly, a heart attack, pulmonary embolus, or aortic dissection, which is like a blister on the aorta that could rupture. A CT can eliminate all three of these prospects in one shot. So, if you come in with chest pain and you get CT angiography and the arteries are clean and vessels look good, then the physician will start to look for other things. CT of the coronary arteries can also be done on an outpatient basis and is less expensive than MRI, and I think that down the road that is going to be the way that all chest pain related algorithms work,” Dr. Church adds.
Although the MRI is lengthier and more expensive, it can provide greater detail of the brain or other organs when a physician is searching for tiny abnormalities. Screening image studies on an preventive basis for either procedure are generally restricted to the evaluation of a specific problem or to diagnose symptoms a patient may be experiencing rather than on a routine basis.
Improvements in Technology
While both MRI and CT technology are relatively recent developments, improvements continue to be made. According to local radiologists and physicians, the procedures are becoming faster and the images are even more startling than those with which diagnosticians have been familiar.
According to Dr. Jason Robertson of the Center for Sports Medicine and Orthopaedics, “The most significant improvement in MRI technology has been the size and strength of the magnet that is used along with the computer interpretation of the images. The increase in the strength of the magnet correlates well with improvement in image quality, which has improved patient care by revealing more intricate detail of the joints and tissues being evaluated.


Whereas before this advancement, a small rotator cuff tear or meniscal tear may not be seen, now the pictures are much more clear. The future advancements in MRI seem to be moving toward improving the speed of the scanning enabling the magnet to capture real-time images for dynamic MRI.”
Dr. Church adds, “The strength of a magnetic field is measured in something called Tesla. The earth’s magnetic field is .09 Tesla, and most of the magnets in use with MRI are 1.5 Tesla. Higher strength Tesla scanners are faster and some as high as 3.0 Tesla are being used. The gradients are much higher in higher strength magnets, so you can see more, like actually looking at the tracks within the brain to see what is going on as neurons form their little pathways through the brain.”
Dr. Quarfordt adds, “The stronger the magnet gets, it becomes almost as clear as what the surgeon sees when he makes an incision, really enhancing the ability to see abnormalities. We have also been able to use MRI instead of an arteriogram of the vessels to the kidneys or legs. MRI is still a little bit slow. We can already do coronary arteries with a CT scan, and if everything looks good we can be 98 percent sure that the vessels to the heart are normal.”


In terms of CT technology, Quarfordt notes that the machine itself resembles a doughnut and that the radiation source and detector on either side have been increased so that fewer rotations are required, the duration of the procedure is shortened, and images are even clearer. “In the old days when CT was new,” he remembered, “it used to take about an hour just to get images out of the machine. Now we can do a picture of a patient’s head in about five seconds.”
Dr. Robertson adds, “The advancements in CT scanning have enabled physicians to view 3D images of fractures and joints to more precisely determine bony anatomy and more accurately assess fracture displacement. This ability to view 3D images of a joint or fracture has improved patient care by helping us to make more informed decisions in regards to treatment planning.
Another advance in CT technology is the development of Positron Emission Tomography (PET), which involves the use of a contrast agent that accumulates in an area where a tumor is present. Therefore, armed with PET-CT images, a physician can locate an area where cancer exists and direct treatment accordingly.
“Also in CT, the coming thing is a 64-slice machine with detectors which are so small and the time so fast that we can image the heart vessels and often replace the need for cardiac catheterization,” says Dr. Church.
With advancements in both technologies, the utilization of both MRI and CT allows physicians to accurately diagnose symptoms, and play a greater role in screening for future medical problems. In both circumstances, the results are higher quality care and better patient outcomes.
Dr. Steve Quarfordt
Chattanooga Imaging
Dr. John Church
Dalton Imaging
Dr. Jason Robertson
Center for Sports Medicine and Orthopaedics

